Esophageal fistula as an infrequent complication of anterior cervical fusion. case report
JOHN VARGAS U., ALFONSO BASURCO C., EDUARDO LAOS P., JESÚS CABREJOS B., RENZO ROMERO
Abstract (Spanish) ||
Full Text ||
PDF (Spanish) ||
PDF (English)
ABSTRACT
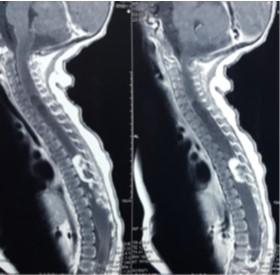
Introduction: The morbidity of anterior cervical fusion surgery is low and one of the least frequent is an esophageal perforation, but this can bring severe complications such as sepsis, mediastinitis, or death. Optimal treatment is multidisciplinary, although it remains controversial; This consists of primary closure or closure by means of a muscle flap, accompanied by rest of the esophagus and a high protein diet.
Clinical Case: A 27-year-old female patient who, after a car accident, presented a cervical vertebromedullary trauma that required posterior cervical decompression surgery followed by stabilization via the anterior approach on 2 occasions. In the postoperative period, she presented erythema in the operative wound, subcutaneous emphysema, and cervical edema, for which she was re-admitted to the operating room being diagnosed with esophageal fistula. Treatment was performed by placing a muscle flap, antibiotics, esophageal bypass, and a high protein diet by nasogastric tube. The clinical and laboratory evolution was favorable, presenting closure of the esophageal fistula.
Conclusion: Esophageal fistula is a rare complication of anterior cervical surgery and this requires multidisciplinary management.
Keywords: Esophageal Fistula, Esophageal Perforation, Sepsis, Decompression, Spinal Fusion. (Source: MeSH NLM)
Evacuation of intracerebral hematomas by Neuroendoscopy: results in a series of cases
JERSON FLORES C.
Abstract (Spanish) ||
Full Text ||
PDF (Spanish) ||
PDF (English)
ABSTRACT
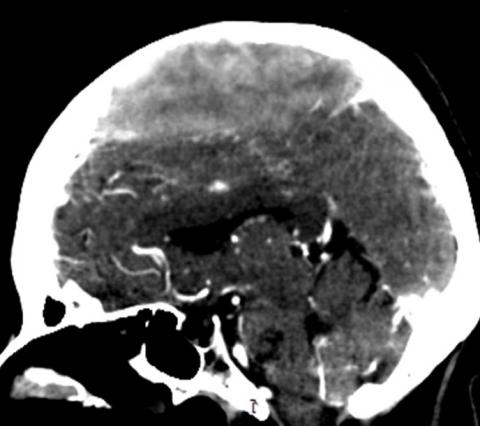
Objectives: Intracerebral (ICH) and intraventricular (IVH) hemorrhage cause severe morbidity and a high mortality rate. Intracranial hypertension and secondary injury in the perihematomal region are associated with a poor prognosis, so early surgical evacuation with minimal damage to brain tissue is essential. Endoscopic evacuation using an Endoport system is a promising technique. The objective of the study is to present the results of the endoscopic evacuation of ICH and IVH in patients operated from 2010-2019 at the Almenara Hospital in Lima-Peru.
Methods: Prospective descriptive study, in a period of 10 years, 48 patients with ICH and IVH underwent endoscopic evacuation in the first 72 hours, using a transparent working channel (Endoport) designed from a 3cc syringe. Postoperative evaluation was done with tomography and neurological follow-up using the Glasgow Coma Scale.
Results: Of a total of 48 cases, 30 were ICH, and 18 were IVH. The most frequent etiology was hypertension (75%), followed by an arteriovenous malformation (19%) and cerebral aneurysm (6%). The most frequent location was the basal nuclei at the putaminal level (29%) and the thalamic region (29%), followed by the subcortical region (17%) and posterior fossa (6%). The evacuation rate was 90% in ICH and 80% in IVH. There were no intraoperative complications, and the most frequent postoperative complication was in-hospital pneumonia (37%). The average time of external drainage in the IVH was 7.6 days. All patients showed improvement in the Glasgow Scale of an average of 4 points (8.8 in the preoperative period to 13.0 in the postoperative period). Overall mortality was 19% (20% in ICH and 16.7% in IVH)
Conclusions: The endoscopic evacuation of an intracranial hematoma is an effective, minimally invasive, and feasible technique to carry out. A modified 3cc syringe can be used as a working channel. This provides enough space for adequate visualization of the hematoma, as well as for the control of intraoperative bleeding.
Keywords: Cerebral Hemorrhage, Hematoma, Endoscopy, Syringes, Intracranial Hypertension. (source: MeSH NLM)
Definitive treatment of cerebral aneurysms at the Cayetano Heredia National Hospital in Lima Peru: a case series results.
GONZALO ROJAS D., JUAN GARAY H., WESLEY ALABA G., CÉSAR RODRIGUEZ C., ROLANDO LOVATON E., RELIX HUAMAN H.
Abstract (Spanish) ||
Full Text ||
PDF (Spanish) ||
PDF (English)
ABSTRACT
Objectives: Subarachnoid hemorrhage (SAH) due to rupture of a cerebral aneurysm continues to be a disease with high morbidity and mortality in our setting, despite advances in microsurgery and endovascular therapy. The objective of the present study was to determine the demography, vascular territory, and complications that occur in the perioperative management of patients with ruptured cerebral aneurysms treated at the Cayetano Heredia Hospital.
Methods: An observational descriptive study of patients with cerebral aneurysm undergoing surgical and endovascular treatment was carried out in the Neurosurgery Service of the Cayetano Heredia Hospital from 2016 to 2018. The clinical records and operative reports were reviewed.
Results: In a period of 30 months, definitive treatment was performed in 56 patients with a diagnosis of a ruptured cerebral aneurysm, of which 5 received endovascular treatment and 51 treatment by craniotomy and clipping. 62.5% were women, and 50% of the total were between the fifth and sixth decade of life. In more than 50% of cases, treatment was performed within 96 hours of SAH. Regarding the affected arterial territory, 15 patients (27%) had an aneurysm of the territory of the anterior communicating (AComA) and another 15 (27%) in the posterior communicating artery (PComA). Mortality was 17.8%, 70% being due to direct causes such as cerebral infarction and severe vasospasm.
Conclusions: The treatment of the aneurysms was mainly by microsurgery, the aneurysms of the AComA, PComA, and middle cerebral (MCA) had a similar proportion and, in more than 50% the treatment was carried out in the first 4 days. More state support is required to increase endovascular therapy and obtain more promising results.
Keywords: Intracranial Aneurysm, Microsurgery, Craniotomy, Endovascular Procedures (source: MeSH NLM)
Complex multiple ruptured aneurysms treated with embolization in a single session: case report.
JOHN VARGAS U., RODOLFO RODRÍGUEZ V., WALTER DURAND C., JESÚS FLORES Q., DANTE VALER G., RICARDO VALLEJOS T., GIANCARLO SAAL Z.
Abstract (Spanish) ||
Full Text ||
PDF (Spanish) ||
PDF (English)
ABSTRACT
Introduction: Multiple aneurysms are responsible for 15 to 35% of spontaneous subarachnoid hemorrhages, some of them being complex aneurysms. These are characterized by their large size, difficult location, wide neck, weak wall structure, giving rise to branches from the aneurysm, presenting calcifications, or due to ineffective previous treatment. Its management is difficult due to the variation in the anatomical distribution and the difficulty of determining which aneurysm is the ruptured one. The complex aneurysm needs special techniques for its management. Embolization has an acceptable complication rate compared to clipping, with the additional benefit of being a minimally invasive technique with a short hospital stay.
Clinical case: A 50-year-old female patient who presented headache, nausea, vomiting, and sensory disorder, being diagnosed with subarachnoid hemorrhage due to a ruptured aneurysm of the bifurcation of the right internal carotid artery. In addition, 3 other aneurysms were found (left carotid bifurcation, top of the basilar, and communicating segment of the left carotid). We proceeded to embolize the two aneurysms of the carotid bifurcation with coils using the remodeling technique, as well as the one at the top of the basilar with coils assisted with a double “Y” stent. The clinical evolution was good, and the patient was discharged without neurological sequelae.
Conclusion: The embolization of multiple aneurysms in a single session is an effective and safe technique. If the aneurysms are complex, the use of "remodeling" techniques or stent assistance is required to achieve a successful outcome.
Keywords: Aneurysm, Ruptured, Subarachnoid Hemorrhage, Embolization, Therapeutic, Stents. (Source: MeSH NLM)
Magnetic Resonance Tractography integrated to Neuronavigation in the surgical planning of a temporal arteriovenous malformation at the Dos de Mayo National Hospital. Case report.
JOSÉ LUIS ACHA S., MIGUEL AZURÍN, ADRIANA BELLIDO.
Abstract (Spanish) ||
Full Text ||
PDF (Spanish) ||
PDF (English)
ABSTRACT
|
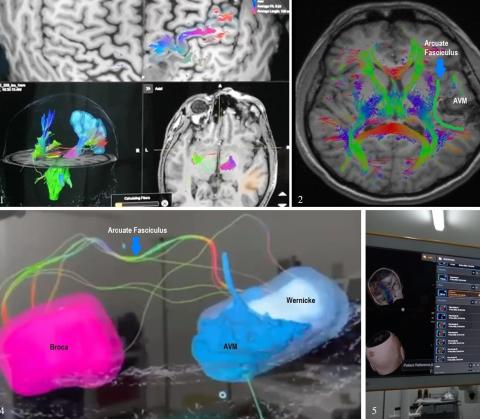
Introduction: Complete resection of a cerebral arteriovenous malformation (AVM) eliminates the risk of bleeding1. Although AVMs that adjoin eloquent areas have been studied with functional neuroimaging or intraoperative mapping, 2 the usefulness of tractography has been limited to case reports or small series. Selecting the patient for surgery for an AVM close to an eloquent area is a challenge. 3
Clinical case: 33-year-old man with a clinical picture of epilepsy for 8 years controlled with carbamazepine. Two years ago, after suspension of treatment, the seizures reappeared, some of the auditory hallucinations "voices asking for help." Brain tomography (CT) showed a hyperdense lesion suggestive of AVM in the left temporal region, which was confirmed with magnetic resonance imaging (MRI) and cerebral angiography. The AVM was completely resected using the tractography integrated into the Neuronavigation.
Conclusion: Magnetic resonance tractography integrated into the Neuronavigation allows to assess in real-time the proximity of the nidus of AVM to the arcuate fasciculus tract and the use of intraoperative fluorescein video angiography allows to assess vascularity in real-time. All of this makes it possible to perform total resection without causing injury to the eloquent area by avoiding compromising the fibers of the arcuate fasciculus tract.
Keywords: Intracranial Arteriovenous Malformations, Neuronavigation, Fluoresceins (Source: MeSH NLM)
|
Intracranial Solitary Plasmacytoma: Case Report
JORGE ZUMAETA S., MANUEL LAZON A., ANNEL MURGA V.
Abstract (Spanish) ||
Full Text ||
PDF (Spanish) ||
PDF (English)
ABSTRACT
Introduction: Solitary intracranial plasmacytoma is a rare plasma cell tumor that affects the skull, meninges, and brain. Unlike multiple myeloma, it does not have systemic manifestations. Its symptoms are characterized by a progressively growing tumor that generates local pain. It does not have a pathognomonic image and can be confused with other lesions, being its diagnosis histological. The prognosis is good and the main treatment modalities are surgery and/or radiation therapy.
Clinical Case: 64-year-old female patient with a clinical picture characterized by loss of strength in lower limbs and thermal rise. On examination: Patient awake, Glasgow 15 points, paraparesis 4/5, photoreactive and isochoric pupils. Imaging examinations show an extensive contrast-enhancing lesion involving cerebral meninges at the frontoparietal level bilaterally, with a moderate mass effect. A subtotal resection of the lesion is performed, with the patient presenting a good clinical evolution. The histological result was a plasma cell tumor. In the 6-month follow-up, no residual lesion was observed, maintaining outpatient control by an outpatient clinic. This case shows a rare pathology that is sometimes confused with a meningioma.
Conclusion: Solitary intracranial plasmacytoma is a rare tumor that can easily be confused with other more common lesions. Its diagnosis is only made with a histological study. It has a good prognosis and can be treated by surgical resection and/or radiotherapy.
Keywords: Plasmacytoma, Brain, Meninges, Neoplasms, Plasma Cell (Source: MeSH NLM)
Advantages of intraoperative videoangiography with fluorescein integrated to the microscope in cerebrovascular pathology. Initial experience at Dos de Mayo National Hospital
JOSÉ LUIS ACHA S., MIGUEL AZURÍN, ADRIANA BELLIDO.
Abstract (Spanish) ||
Full Text ||
PDF (Spanish) ||
PDF (English)
ABSTRACT
|
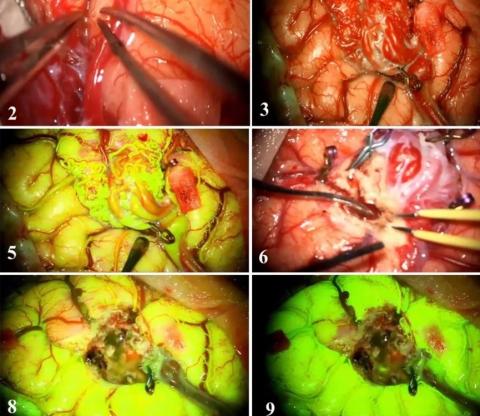
Introduction: Fluorescein sodium (FNa) is a fluorescent substance used to evaluate cerebral blood flow. We present our first cases of vascular microsurgery using microscope-integrated intraoperative fluorescein video angiography. We review the practical applications and benefits of this technique in vascular microsurgery.
Clinical cases: A 63-year-old woman, Glasgow: 9 on admission, with subarachnoid hemorrhage (SAH) Fisher IV. A ruptured anterior communicating aneurysm was diagnosed. After stabilization in the ICU, she underwent surgery, undergoing microsurgical clipping guided by intraoperative videoangiography. The postoperative evolution was favorable.
A 33-year-old man with a history of epilepsy on carbamazepine treatment. After suspension and irregular treatment 2 years ago, seizures reappear. An angiography and magnetic resonance imaging were performed, and he was diagnosed with a left posterior temporal arteriovenous malformation (AVM) close to Wernicke's area, for which he underwent surgery using tractography and videoangiography in real-time integrated into Neuronavigation. In both cases, the benefits of using the integrated microscope were observed thanks to the vascular anatomical assessment in real-time with fluorescein.
Conclusion: Videoangiography with FNa allows examining afferent and efferent vessels during surgery for arteriovenous malformations, checking the persistence of flow in a microvascular anastomosis, and evaluating flow during clipping of an aneurysm. It has the advantages of being able to be repeated during surgery, allowing surrounding anatomical visualization, as well as allowing any surgical correction in real-time.
Keywords: Fluorescein Angiography, Microsurgery, Aneurysm, Arteriovenous Malformations (Source: MeSH NLM)
|
Transsphenoidal endoscopic surgical treatment of pituitary tumors at the Cayetano Heredia National Hospital in Lima Peru: outcomes of a series of cases
JUAN GARAY H, GONZALO ROJAS D, WESLEY ALABA G, JERSON FLORES C, RÓMULO RODRIGUEZ C, YVAN SALCEDO F.
Abstract (Spanish) ||
Full Text ||
PDF (Spanish) ||
PDF (English)
ABSTRACT
Introduction: In recent years, transsphenoidal endoscopic surgery has become a surgical procedure of choice for the treatment of pituitary tumors. The objective of the present study was to describe the demographic, clinical characteristics, complications, and postoperative results of the patients who underwent transsphenoidal endoscopic resection.
Methods: A descriptive case series study of patients with pituitary tumors operated through a transsphenoidal endoscopic approach was carried out from January 2016 to August 2018 in the Neurosurgery Department of the Cayetano Heredia National Hospital. Data were obtained by reviewing the medical records.
Results: A total of 20 endoscopic surgeries were performed, of which 08 were for pituitary macroadenomas, 07 for giant pituitary adenomas, and 05 for other tumor lesions. Of the total number of operated patients, 11 were male (55%) and the most frequent age group was between the 3rd to 5th decade of life (70%). Regarding the postoperative results, a total and subtotal resection was performed in 60% of the patients and partial resection in 20%. Regarding postoperative complications, 45% of patients had transient diabetes insipidus. 1 patient died (5%) due to septic symptoms.
Conclusions: Endoscopic transsphenoidal surgery provides several advantages over microscopic transsphenoidal surgery, such as providing greater anatomical detail, direct visualization of the tumor, and cerebrospinal fluid leak sites, which allows achieving better results in terms of disease control and the prevention of complications. However, studies with a larger number of patients are necessary.
Keywords: Pituitary Neoplasms, Endoscopy, Neurosurgical Procedures, Diabetes Insipidus. (source: MeSH NLM)
Endoscopy-assisted microsurgery in the resection of epidermoid tumor of the pontocerebellar angle
JERSON FLORES C., GONZALO ROJAS D., WESLEY ALABA G., RÓMULO RODRIGUEZ C.
Abstract (Spanish) ||
Full Text ||
PDF (Spanish) ||
PDF (English)
ABSTRACT
Introduction: Intracranial epidermoid tumors are rare, slow-growing, and histologically benign congenital neoplasms. The microsurgical approach with endoscopic assistance is described as a minimally invasive technique that facilitates the work of the neurosurgeon in the complete resection of an epidermoid tumor located in the cerebellopontine angle.
Clinical Case: 62-year-old woman, with a 3-year disease characterized by pain on the right side of the face. Symptoms increase in the following 2 years, becoming disabling and only partially improving with pregabalin and oxcarbazepine. Brain MRI showed a hypointense lesion with a cystic appearance at the level of the prepontine cistern with expansion to the right cerebellopontine angle that compressed the right trigeminal nerve (V). Retromastoid craniotomy and a right cerebellopontine angle approach were performed. Under the microscopic vision, the trigeminal nerve was identified which was pulled by the tumor, the cranial nerve complex VII-VIII, and vessels such as the superior petrous vein and the anteroinferior cerebellar artery. With the support of the endoscope, the tumor was better visualized in inaccessible areas, the prepontine cistern was accessed and total resection of the tumor was achieved. The patient evolved favorably with remission of pain on the right side.
Conclusion: The microsurgical technique assisted by endoscopy allows safe removal of the tumor, and it is immensely helpful in the resection of tumors from regions not visible under the microscope.
Keywords: Brain Neoplasms, Trigeminal Nerve, Endoscopy, Cerebellopontine Angle. (source: MeSH NLM
Microsurgical resection of a pontine cavernoma through a far lateral infratentorial supracerebellar approach
CARLOS VASQUEZ P., GONZALO ROJAS D., JOSÉ CALDERÓN S., YELIMER CAUCHA M.
Abstract (Spanish) ||
Full Text ||
PDF (Spanish) ||
PDF (English)
ABSTRACT
Introduction: Cavernomas on the posterolateral pontomesencephalic surface can be approached from an extreme lateral supracerebellar infratentorial corridor, although the theory is scarce. The brainstem has a dense concentration of nuclei and fibers that are responsible for a high rate of morbidity when treating brainstem lesions. The objective of this work is to demonstrate the safe microsurgical resection technique for the complete removal of a pontine cavernoma.
Clinical Case: 27-year-old woman with a 5-month history of disease; characterized by headache, left facial paresis, and right half body paresis. Magnetic resonance imaging (MRI) showed a hemorrhage in the middle cerebellar peduncle compatible with a ruptured cavernoma, initially receiving medical treatment. Subsequently, due to an increase in the motor deficit and the presence of keratopathy in the left eye, surgery was decided. A retromastoid craniotomy and an extreme lateral supracerebellar infratentorial approach were performed. A safe entry zone was identified and the cavernoma was completely excised. In the postoperative period, she did not present additional neurological deficit, being extubated at 24 hours, with a score on the Glasgow scale of 15 points. Postoperative brain tomography (CT) showed the absence of the cavernoma.
Conclusion: The far lateral supracerebellar infratentorial approach is safe for the excision of cavernomas with a middle cerebellar peduncle. When combined with the significant reverse Trendelenburg position it results in minimal cerebellar retraction as the cerebellum descends with gravity.
Keywords: Hemangioma, Cavernous, Pons, Middle Cerebellar Peduncle, Craniotomy (source: MeSH NLM)
Intracerebral hematoma caused by Moyamoya disease: a case report
JOHN VARGAS URBINA, GIANCARLO SAAL Z., FERNANDO PALACIOS S.
Abstract (Spanish) ||
Full Text ||
PDF (Spanish) ||
PDF (English)
ABSTRACT
Introduction: Moyamoya disease is a chronic occlusive cerebrovascular disease of unknown etiology, characterized by bilateral stenotic and occlusive changes in the terminal portion of the internal carotid, as well as the presence of an abnormal vascular network at the base of the brain. The diagnosis is made with magnetic resonance (MRI) and digital subtraction angiography (DSA), SPECT is useful in the therapeutic decision. The surgical treatment of choice is revascularization.
Clinical Case: A 50-year-old female patient from China, with the Glasgow Coma Scale (GCS) of 9, and a clinical picture of stroke. An admission brain tomography (CT) revealed a right temporal hematoma. Surgical evacuation of the intracerebral hematoma was performed. Cerebral angiography revealed distal stenosis of the internal carotid artery and its branches, being diagnosed with Moyamoya disease. The evolution was favorable, neither a motor deficit nor a decreased level of consciousness (GCS:15) was observed at the time of discharge. A subsequent revascularization surgery was indicated.
Conclusion: Moyamoya disease is a rare cause of intracerebral hematoma but should be suspected in adults of Asian descent. MRI and angiography are the diagnostic methods of choice. Surgical treatment is revascularization, which improves the prognosis.
Keywords: Moyamoya Disease, Cerebral Hemorrhage, Stroke, Cerebral Angiography (Source: MeSH NLM)
Tension pneumocephalus after surgical evacuation of chronic subdural hematoma: case report and pathophysiological mechanism
FERNANDO CELI, GIANCARLO SAAL Z.
Abstract (Spanish) ||
Full Text ||
PDF (Spanish) ||
PDF (English)
ABSTRACT
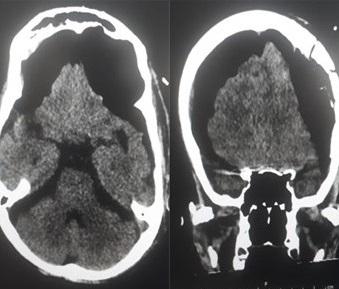
Introduction: Pneumocephalus is a frequent complication following neurosurgical procedures. The diagnosis is based on tomographic findings and the clinical evolution of the patient. Therefore, we detail the physiopathological mechanisms that trigger this complication.
Clinical Case: We present the clinical case of an 85-year-old man who underwent a keyhole craniotomy and subdural drainage placement due to the diagnosis of a chronic subdural hematoma (CSDH) and subsequently developed sudden tension pneumocephalus which triggered the death of the patient due to intracranial hypertension.
Conclusion: Tension pneumocephalus is a life-threatening complication that must be suspected early and must be treated as an emergency.
Keywords: Hematoma, Subdural, Chronic, Pneumocephalus, Drainage, Craniotomy (Source: MeSH NLM)
Extramedullary intradural capillary hemangioma in a patient of 03 months of life: a case report
JOSÉ LUIS URQUIZO, ALFONSO BASURCO C, WILLIAM ANICAMA, ROCÍO TORRES
Abstract (Spanish) ||
Full Text ||
PDF (Spanish) ||
PDF (English)
ABSTRACT
Introduction: Capillary hemangioma is an extremely rare endothelial cell neoplasm as an extramedullary intradural tumor. Its presentation in infants is anecdotal and only 2 cases have been previously reported in the literature.
Clinical case: a 03-month-old infant with severe abrupt-onset paraparesis. Spinal magnetic resonance imaging (MRI) showed an intraspinal tumor at the T7, T8, and T9 levels, which captures contrast. A T7-T9 laminectomy and microsurgical resection of the extramedullary spinal tumor were performed. The pathology was reported as lobulated angiomatous proliferation with focal vascular thrombus, with positive immunohistochemistry for CD 31 and 34, compatible with capillary hemangioma. The neurological evolution was favorable. Post-surgical MRI and spinal angiography showed little residual tumor and hydrosyringomyelia in remission.
Conclusion: Capillary hemangioma is a rare pathology in infants, this case being the 3rd case reported. Its diagnosis and surgical resection are important since most patients present an improvement in the neurological deficit after surgery. Surgical treatment avoids the risk of acute bleeding
Keywords: Hemangioma, Capillary, Spinal Cord Neoplasms, Infant, Laminectomy. (Source: MeSH NLM)
Neurosurgical treatment of unstable cervical spine due to rheumatoid arthritis: case series
JORGE ZUMAETA S, ELAR CARI C, ALFONSO BASURCO C, CESAR POLO D, JESUS CABREJOS B, PABLO PINO L, JUAN SALAS G, EDUARDO LAOS P, ROBERT BURGOS C.
Abstract (Spanish) ||
Full Text ||
PDF (Spanish) ||
PDF (English)
ABSTRACT
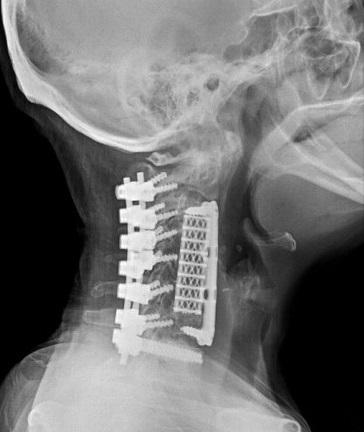
Introduction: Rheumatoid arthritis (RA) is a systemic disease characterized by synovitis, which causes damage to the ligaments and joints. The cervical region is the region of the spine most affected, with neck pain the most frequent symptom. The three forms of presentation are atlantoaxial subluxation, cranial settlement, and subaxial subluxation. The clinical evolution of patients treated conservatively is poor, with surgery being a key element to prevent the progression of neurological deterioration.
Methods: A retrospective study of 10 patients with RA operated between 2015 and 2019 was carried out. Ranawat criteria were used for clinical classification and imaging studies were performed to confirm cervical instability. Anterior and posterior cervical arthrodesis techniques were used. Control after surgery was performed by tomography and the Ranawat score was determined in the outpatient control.
Results: In the period 2015 and 2019, 10 patients with RA who presented symptoms of cervical instability were operated on. All patients were female, aged between 52 and 73 years. The most frequent symptom was neck pain. Most of the patients presented inflammatory markers (ESR, CRP) in high values. The most frequent cervical involvement was atlantoaxial instability. The most common surgical technique used was posterior C1-C2 arthrodesis via the inter-articular approach. Ranawat's classification improved in 90% of patients after surgery. Complications were surgical site infections and rupture of occipitocervical fixation bars, which were adequately resolved.
Conclusions: Surgery for patients with vertebral instability due to RA should be aimed at treating intractable pain and stopping the progression of cervical instability, with the aim of promoting neurological recovery and reducing mortality.
Keywords: Spine, Arthritis, Rheumatoid, Joint Instability, Synovitis, Neck Pain, Arthrodesis. (source: MeSH NLM)
Recurrent lumbar disc prolapse, causative factors and outcome in bangladeshi people
MOSHIUR RAHMAN, MD, EZEQUIEL GARCIA-BALLESTAS, MD, LUIS RAFAEL MOSCOTE-SALAZAR, MD
Abstract (Spanish) ||
Full Text ||
PDF (Spanish) ||
PDF (English)
ABSTRACT
Introduction: Recurrent lumbar disc prolapses (RLDP) is not uncommon after surgery. The incidence of RLDP varies from 5-18% across the different populations in the world. The exact cause of recurrence is not known but the weakness of the annular tissue due to previous surgery, exposure to repetitive lifting, heavy work causing axial load, advanced age, smoking, are some of them. RLDP can be managed conservatively, but if that fails, such cases are candidates for surgery. Various surgeries can be done- open versus minimally invasive surgeries, fusion versus non-fusion surgeries are debatable. The study aims to evaluate the causative factors of RLPD and the outcome of surgeries in Bangladeshi peoples.
Methods: A total of 126 cases of RLDP in 1800 lumbar disc surgery patients were included in the study. This study was retrospective and multicenter data were analyzed from 4 private hospitals. The male-female ratio was 3:2. The study period was from 2009 to 2018. The Minimum follows up period was 1 year.
Results: There was a significant risk of RLDP in sex, smoking habit, BMI, and heavy workers. By using these differences, a logistic regression analysis showed that males increased BMI, heavy workers, residual disc particularly under posterior longitudinal ligament, indiscipline life, and smoker could predict lumbar disc herniation recurrence. Minimally invasive surgeries had better outcomes than open surgical methods. Fusion surgeries with stabilization were encouraging.
Conclusions: Patients who are male, increased BMI, heavy workers, indiscipline life, and smoker could predict lumbar disc herniation recurrence. Minimally invasive surgeries under illumination have a better outcome than open surgical methods. Residual disc, particularly under posterior longitudinal ligament, is associated with a high recurrence of symptoms. Patient selection, clinical examination, investigations, and understanding the indications for surgery in recurrent cases is the key to success.
Keywords: Lumbar, Disc, Prolapse, Recurrence (source: MeSH NML)