Usted está aquí
Peruvian Journal of Neurosurgery
Acute pneumocephalus in neurosurgical patients operated on in supine and prone position
ABSTRACT
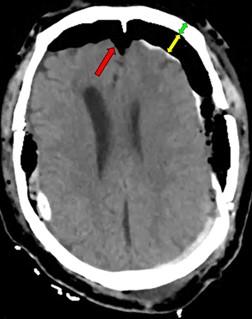
Objectives: To determine the incidence, associated factors, distribution, and degrees of acute post-surgical pneumocephalus in patients with cranioencephalic pathology operated on in the supine and prone position.
Methods: Observational, prospective, and cross-sectional study in patients 18 years of age or older, with cranioencephalic pathology belonging to the Neurosurgery Service of the Cayetano Heredia National Hospital, March 2022 - February 2023. All were operated in the supine or prone position. Acute (<= 72hrs) post-surgical pneumocephalus was identified by brain tomography. Those with pre-surgical pneumocephalus and operated on in positions other than supine and prone were excluded.
Results: Of 100 patients with cranioencephalic pathology who underwent surgery in the supine and prone position, 54% were male and 56% were under 60 years of age. In addition, 56% presented some comorbidity, and 54% had non-traumatic cranioencephalic pathology. The entire population presented some patterns of distribution and degree of postoperative acute pneumocephalus. There were no deaths from pneumocephalus. There was an association (p<0.005) between some distributions of pneumocephalus with the female sex, traumatic cranioencephalic pathology, and the creation of a surgical access to some intracranial space. In the same way, an association (p<0.005) was evidenced between the degrees of pneumocephalus of some intracranial space with the surgical opening towards this or another deeper space.
Conclusions: Acute post-surgical pneumocephalus is frequent in patients with cranioencephalic pathology operated on in supine and prone positions. The distribution and degrees of pneumocephalus may be related to sex, the type of cranioencephalic pathology, and the depth of the surgical lesion.
Keywords: Pneumocephalus, Prone Position, Intraoperative Complications, Neurosurgery. (Source: MeSH NLM)
Neurobiological basis of behavior. Is it possible to change a human being?
ABSTRACT
|
Knowledge of the neurobiological bases of behavior, and above all, mastery of the tools necessary for its modification, is essential for addressing numerous types of pathologies with clinical and social impact. Outside of the clinical setting, the prison rehabilitation system has arguably been the most neglected throughout the history of the republic in our country. Promoting innovative alternatives under the full weight of scientific evidence is a clear path to progress, thereby generating a better society, addressing the undeniable rise in the crime rate we all face every day. Shaping neurogenesis through enriched environments is a tool with promising results. People can change; we only need to change our approach to offer them even a chance for the common good of society. Keywords: Medicine, Social Change, Social Justice, Humans (source: MeSH NLM) |
Combined half and half pretemporal and subtemporal approach for petrous apex meningiomas with projection to the infratemporal fossa and petroclival region: surgical technique and outcome
ABSTRACT
Introduction: Petrosal apex meningiomas are defined as tumors originating in the petrous angle and which may extend anteriorly, extending from the infratemporal region to the petroclival region. Total resection of petrous apex tumors has been considered to carry a high risk of mortality and neurological sequelae. We present the first case performed at the Hospital Nacional PNP Luis N. Sáenz using a combined pretemporal and subtemporal approach for petrous apex meningiomas projecting to the infratemporal fossa and petroclival region.
Case Report: A 55-year-old male patient with no medical history presented with a 2-year history of headache, bitemporal hemianopia, tinnitus, and paresthesias on the left side of the face. A combined half-and-half pretemporal and subtemporal approach with an infratemporal fossa projection was performed, achieving complete tumor resection and preservation of cranial nerve function, without intraoperative complications. The patient progressed favorably without a significant neurological deficit and was discharged on the 8th day.
Conclusion: The combined half-and-half pretemporal and subtemporal approach with an infratemporal fossa projection for meningiomas arising in the petrous apex with extra-axial and intradural projection and extending into the petroclival region is an effective option for the resection of highly complex tumors.
Keywords: Meningioma, Petrous Bone, Hemianopsia, Infratemporal Fossa. (Source: MeSH NLM)
Postoperative recurrence of intramedullary intraspinal Neuroenteric cyst: case report.
ABSTRACT
Introduction: Neuroenteric cysts (NECs) are rare, congenital, and benign lesions that result from persistent or abnormal communication between the neuroectoderm, notochord, and endoderm. They occur primarily in pediatric and young adult patients and are associated with other vertebral-medullary, gastrointestinal, and respiratory malformations. They are intradural, extramedullary lesions, with intramedullary presentation being rare. We present the case of a patient with a recurrent intramedullary intraspinal Neuroenteric cyst at the D4-D5 level.
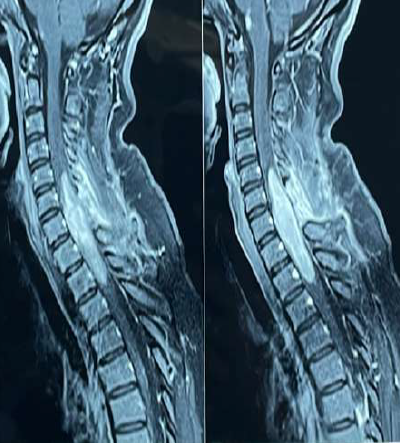
Clinical case: A 39-year-old male patient with a history of spinal surgery for intramedullary cysts on two occasions presented with a 1-month history of moderate-intensity stabbing pain in the thoracic region radiating to the anterior region of dermatome T4, associated with predominantly left-sided paraparesis and bladder and rectal sphincter disturbances. Magnetic resonance imaging (MRI) of the cervical spine showed a hypointense cystic tumor on T1 and hyperintense on T2 at the T4-T5 level, consistent with an intramedullary Neuroenteric cyst. On examination, the patient was awake, with a Glasgow Coma Scale of 15, isochoric, photoreactive pupils, predominantly left-sided paraparesis (LLL 3/5, RLI 4/5), sensory level T5, and left patellar hyperreflexia. A T4 and T5 laminectomy was performed with evacuation of the intramedullary cyst and placement of a cysto-subarachnoid shunt, without complications. The patient's postoperative clinical course was favorable, showing recovery of motor deficits.
Conclusion: Surgical resection is the treatment of choice for Neuroenteric cysts. The goal should be total resection due to the high recurrence rate. A follow-up MRI is recommended for subtotal resections.
Keywords: Cysts, Neural Tube Defects, Neural Plate, Laminectomy. (Source: MeSH NLM)
Isolated spinal Rosai-Dorfman disease: Presentation of a recurrent case and review of literature
ABSTRACT
Introduction: Rosai-Dorfman disease, also known as sinus histiocytosis, is a proliferative process characterized by painless lymphadenopathy and metabolic disorders. Central nervous system (CNS) invasion is uncommon (5%), and an isolated variant occurs in only 0.5%. Symptoms such as paresis and sensory disturbances are more frequent in the thoracic spine. Magnetic resonance imaging (MRI) is fundamental for diagnosis, which is confirmed by histopathology and immunohistochemistry studies. Surgical resection is the therapy of choice.
Clinical case: An adult female patient with no significant medical history presented with a 9-month clinical picture characterized by progressive weakness in the lower limbs. Upon examination, she was awake with left hemiparesis and preserved sensation. A cervicodorsal MRI showed an intraspinal cystic lesion within the C1-C5 spinal cord with signs of spinal cord edema and increased volume. Posterior cervical surgery with subtotal excision of the intramedullary tumor was performed. Postoperatively, the patient's clinical course was stable with quadriparesis predominantly in the lower limbs. However, in 3 months, increased paresis and sphincter disturbance were evident, leading to further surgery. Pathology and immunohistochemistry results revealed Rosai-Dorfman disease.
Conclusion: Rosai-Dorfman disease of the central nervous system (CNS) is a rare, benign disorder that can cause spinal cord invasion and spinal cord compression, resulting in paresis or sphincter disturbance. The presence of a contrast-enhancing lesion on MRI is mandatory for determining the option for surgery, and histopathological examination is essential for confirmatory diagnosis.
Keywords: Histiocytosis, Sinus, Spinal Cord Compression, Paresis, Central Nervous System (Source: MeSH NLM)
Primary amoebic meningoencephalitis due to Naegleria fowleri: case report.
ABSTRACT
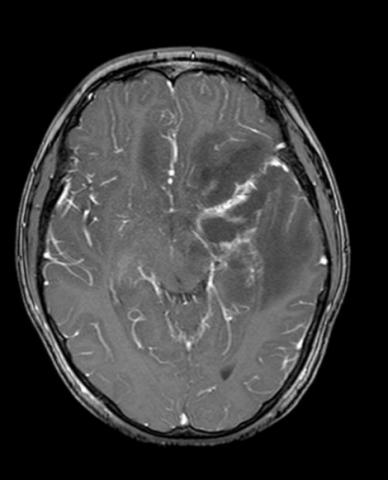
|
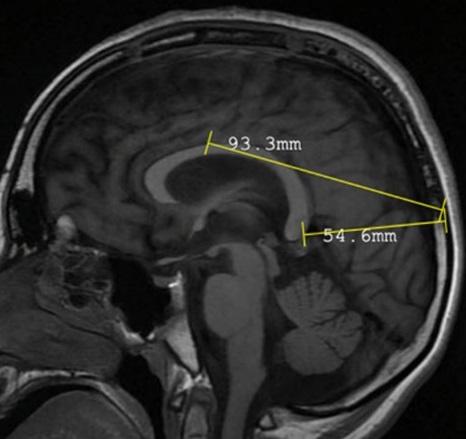
Objective: Free-living amoeba infections present with acute intracranial hypertension that are difficult to manage. In Peru, the most reported species are Balamuthia spp., Acanthamoeba spp., and Naegleria spp. We present the case of a child with a torpidly progressing amoebic meningoencephalitis, seen in our hospital in May 2023. Our objective is to describe the aggressive clinical presentation as a differential diagnosis for a brain tumor. Clinical case: A 9-year-old male patient from rural northern Peru with a history of protein malnutrition presented with an initial clinical presentation of mild headache, progressive weakness in the right side of the body, subsequently progressing to severe headache, vomiting, and neurological deterioration. Examination revealed drowsiness, global aphasia, right hemiplegia, and left ptosis. Three surgeries were performed in two stages: First, a left frontotemporal craniotomy and partial excision of a poorly defined, yellowish lesion attached to the neurovascular structures of the Sylvian valley; second, a left decompressive craniotomy and external ventricular drainage for severe intracranial hypertension. Conclusion: Treatment of cerebral amebiasis should be multidisciplinary. Early initiation of specific drugs is crucial to reduce mortality and complement surgical and intensive care treatment, given the aggressive nature of the infection. Keywords: Amebiasis, Amoeba, Naegleria, Intracranial Hypertension, Hemiplegia. (Source: MeSH NLM)
|
Endovascular treatment with coils of aneurysm of the anterior communicating artery, angiographic control, and evolution according to packing density: case series.
ABSTRACT
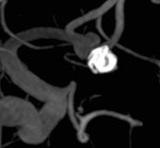
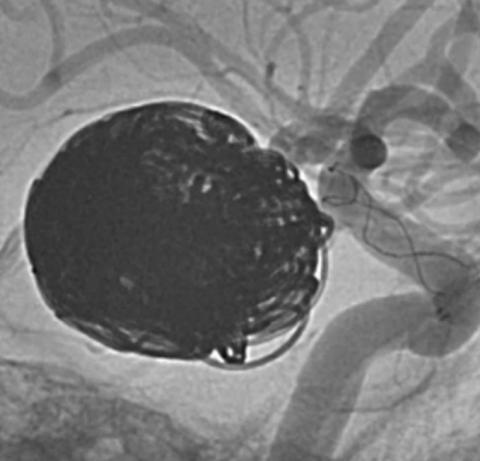
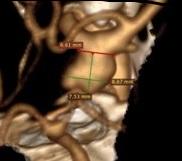
Giant unruptured posterior communicating segment aneurysm embolized in one session with stent and coils.
ABSTRACT
Aneurysms and other intracranial lesions in polycystic kidney disease: illustrative case and review
ABSTRACT
Selective posterior corpus callosotomy in a child with Lennox–Gastaut Syndrome: case report
ABSTRACT
Central diabetes insipidus post-ventriculostomy. case report
ABSTRACT
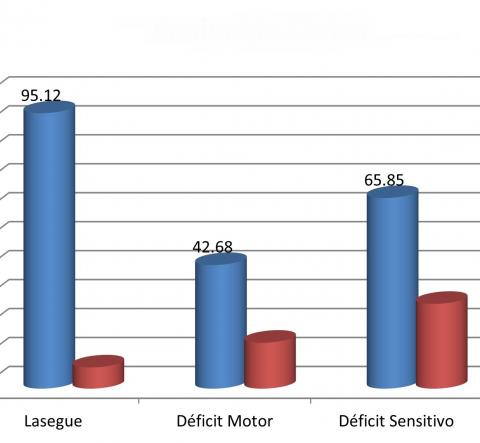
Experience in lumbar microdiscectomy at the Guillermo Almenara Irigoyen Hospital 2018 -2021
ABSTRACT
Beginnings of endoscopy spine surgery in Peru
ABSTRACT
|
In recent years, spinal endoscopy has become increasingly common in our setting; however, its use is not recent. The first reported cases date back to the early 2010s by a team from the Cayetano Heredia Hospital in charge of Drs. Wesley Alaba and Jerson Flores. Although other minimally invasive procedures such as nucleoplasty, nucleolysis, or percutaneous rhizotomies had already been used since the 2000s, it was not until 2011 that endoscopy was used for the first time in a standardized manner in spinal surgery with the endoscope as the only element of vision, successfully resecting a vertebral lesion.
The first cases of vertebral pathology in which endoscopic surgery was used were the resection of a synovial cyst and a tuberculous abscess, followed by the resection of herniated discs at the L5-S1 level and later at the L3-L4 and L4-L5 levels. The first approach was the tubular interlaminar posterior approach, followed by the transforaminal endoscopic approach and the percutaneous posterior interlaminar approach. In the following years, endoscopy has been used not only in resecting herniated discs but also in treating central and lateral canal stenosis, reaching significant experience in this technique.
The development of spinal endoscopy and its increasingly widespread use by neurosurgeons and traumatologists from different hospitals in the country represents an important advance in spinal surgery in Peru, which brings greater benefit to patients.
Keywords: Endoscopy, Intervertebral Disc Displacement, Endoscopes, Neurosurgeons (source: MeSH NLM)
|
Spinal tuberculosis: a diagnostic challenge. case report and literature review
ABSTRACT
|
Introduction: Spinal tuberculosis TB represents 1% of all TB cases and 50 - 60 of osteoarticular TB cases.1 Certain atypical clinical and radiological presentations of spinal tuberculosis are described infrequently. 2 The lack of recognition of these presentations can lead to a delay in diagnosis and in the initiation of treatment. 3 We present the case of a patient with atypical vertebral tuberculosis operated on in our hospital.
Clinical case: A 56-year-old male with a history of diabetes mellitus no history of tuberculosis contact with a 3-year history of moderate low back pain without sciatic pain that did not improve with physical therapy The general and systemic physical examination was normal The tests showed PCR 9.8 ESR 24 BK in sputum brucellosis test and ELISA and chest X-ray were normal. A tomography and magnetic resonance imaging of the lumbosacral spine showed an osteolytic lesion involving L2 L3, isointense on T1 with regular punched-out borders sparing the L2 L3 intervertebral disc suggestive of vertebral tuberculosis He received standard tuberculosis treatment for 24 months with no improvement A new open biopsy revealed Mycobacterium tuberculosis GenXpert.
Conclusion: Spinal tuberculosis continues to be a global health problem Diagnosing atypical spinal tuberculosis remains difficult which could lead to inappropriate treatment especially regarding the choice of treatment regimens and surgical options Histopathological confirmation is essential for time management
Keywords: Tuberculosis, Spinal, Mycobacterium tuberculosis, Lumbar Vertebrae, Biopsy (Source: MeSH NLM)
|