Usted está aquí
Peruvian Journal of Neurosurgery
Epidemiology of traumatic brain injury in children
ABSTRACT
Stereotactic Radiosurgery: Gamma Knife or Linac?
ABSTRACT
Objective:To investigate Gamma Knife and LINAC radiosurgery technologies regarding technical aspects and clinical results.
Patients and methods: A comparison was made with respect to stereotactic frame, mechanical accuracy, dosimetry, radiobiology, treatment planning and clinical results regarding both systems.
Results: The different stereotactic frames available in the market are not different in terms of proper fixation as well as for geometric localization reference. Similar excellent clinical results are obtained for small lesions with photon beams of the gamma knife and the linac. Similar beam dose distributions with sharp fall-off for small spherical shaped targets are obtained for both devices. The superior mechanical precision for the gamma knife as compared with the linac is of limited clinical relevance because inaccuracy of cranial target localization based on contemporary available radiological imaging is greater than the typical linac imprecision (of around 1mm). Treatment planning systems for the linac are not standardized but are based on well-known algorithms. The linac has no field size limitations, achieving more homogeneous dose distributions compared with that obtained with the gamma unit.
Conclusion: Linac based radiosurgery is a practical treatment method with equivalent physical, radiobiological and clinical results compared to the gamma knife technology although its routine methodology requires multidisciplinary effort
Skull base approaches: Brief revision (I part)
ABSTRACT
Surgical approachs to the skull base are usefull in the treatment of expansive and vascular lesions that localize there or near there, increasing significantly the exposition and reducing the need for brain retraction with minor risks of injury during their resection. This is a brief revision of the main approaches to the skull base that describes surgical techniques of them, taking as a reference the experience gained by the autor in a course directed by Dr. Antonio Bernardo, in Anspach®´s laborartories, thanks to a scholarship sponsored by Neurosurgical Peruvian-American Foundation and Peruvian Neurosurgical Society.
Primary central nervous system lymphoma: Case report
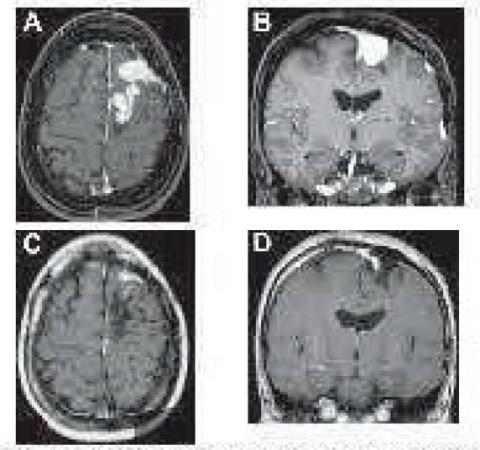
ABSTRACT
Primary central nervous system lymphoma (PCNSL) is a rare form of non-Hodgkin lymphoma (NHL) which affects brain, spinal cord, leptomeninges and eyes. Its clinical course and radiological features are different in inmunocompetent patients comparated with inmunocomprised patients, especially in patients with acquired inmunodeficiency syndrome (AIDS). The diagnosis should be followed for a detailed evaluation, including a carefully physical examination, ophthalmologic evaluation, a chest/abdomen/pelvis computed tomography (CT) scan, cerebrospinal fluid (CSF) analysis, human immuno deficiency virus (HIV) testing and a contrast enhanced brain magnetic resonance image (MRI). MRI usually shows one or more enhanced paraventricular lesions, deep in the white matter, spanning the corpus callosum. Stereotactic brain biopsy sampling is the gold standard for the diagnosis. The use of Metotrexate in high doses followed by radiotherapy has demonstrated the best results in the treatment of PCNSL. A 44 years old woman, with apparently spontaneous remission of multiple brain lesions demonstrated in MRI plus initial negative biopsy sampling for PCNSL, showed tumoral enlarging after a follow up of 2 years.
Surgical treatment of carpal tunnel syndrome by minimally invasive non endoscopic technique (MINET)
ABSTRACT
We present the anatomical considerations that support a surgical alternative designed for the surgical treatment of Carpal Tunnel Syndrome (CTS). The design of the technique maintains the concept of minimally invasive and at the same time the one of not requiring the use of endoscope. The results obtained in the last 100 cases are presented.
Epidemiological Analysis of Neurosurgical Patients in the Intensive Care Unit
ABSTRACT
The care of neurosurgical patients in intensive care units has proven to be beneficial not only for patients but also for hospital institutions. However, the benefits of the care that these units provide to the neurocritical patient depend on multiple factors intrinsic to the patient, which should be studied in order to make better use of resources in the care of them. The present descriptive work shows an analysis of the characteristics of the patients admitted by the specialty of Neurosurgery to the Intensive Care Unit of the Ricardo Palma Clinic during 2007, and a total of 115 patients were studied.
The most common pathologies were: ischemic stroke (37%), intracerebral hemorrhage (17%), and brain tumor (13%). %). The mean length of stay in the ICU was 4.7 days +/- SD 6.6, ranging from 4.3 days for stroke to 11.0 days for a polytrauma patient. The overall mortality found for the neurosurgical patient was 13 per 100, being higher in patients with intracranial hemorrhage (25 per 100). The readmissions and complications of these patients were minimal.
Stereotactic Radiosurgery in Intracranial Meningioma
ABSTRACT
The meningioma has the second place in frequency between the intracranial tumors. The best treatment is complete surgical resection with resection of its dural insertion and areas of cranial invasion. In many cases this goal can be reached with minimal and reasonable morbidity, but in others, and despite the recent advances in microsurgical techniques, the eloquence of the region where the tumor sits leads to morbidity rates of 12 to 30% or to resection In order to preserve neurological function. In those cases in which complete resection can be achieved, the recurrence rates expected at 5 and 10 years are 5 and 10%, respectively. Usually, after microsurgery, some modality of radiation therapy is indicated for the management of the residual tumor, be it radiosurgery based on linear accelerator or LINAC, gamma knife, proton beams or conventional fractional external radiotherapy.
At present, due to its high rate of tumor control and low complications, stereotactic radiosurgery has become a reasonable therapeutic alternative, especially for meningiomas of the skull base. In the present article we briefly review the results of microsurgery and radiosurgery in its aspects of indications, radiobiology, dosimetry, and results.
Clinical practice guide of Infections and infestations of the Central Nervous System
ABSTRACT
Infectious diseases and infestations are due to the local aggression of the central nervous system and its envelopes, by microbial or parasitic agents, capable of causing damage to our health, causing local and general symptoms.
CRANE AND BRAIN PATHOLOGY GROUPS:
Abscess or epidural empyema
Subdural empyema or abscess
Abscess or intracerebral empyema
Ventriculitis
GROUPS OF COLUMN AND MEDULA PATHOLOGY SPINAL AND SPINAL CORD
Abscess or epidural empemema
Subdural empyema or abscess
Abscess or intramedullary start
NERVOUS SYSTEM CYSTICERCOSIS
Cysticercosis Racemosa
Cysticercosis Cystic
Obstructive Hydrocephalus
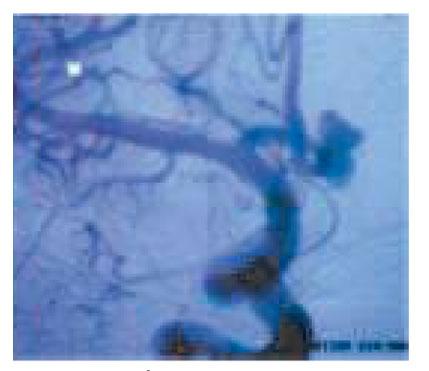
Anterior communicating artery aneurysms: Management and statistic
ABSTRACT
In this prospective study, the authors report their recent experience with 28 patients, using a combined surgical and endovascular team for the management of ACoA aneurysms from 2000 to 2007. Patients were divided into group A, which included 24 Micro surgical patients (18 of them with subarachnoid hemorrhage, group A1, and 6 with unbroken aneurysms, group A2); And group B, consisting of 4 patients treated with GDC embolization. The proposed treatment was based on the direction of the aneurysm fundus projection, the patient's physiological status, treatment risk, aneurysm neck size and Hunt and Hess classification.
The morphological results were analyzed by performing routine angiography and CT. Excellent outcome (GOS score 5) was observed in 16 (72.2%) among 22 patients with good preoperative grade. Group A1 had permanent morbidity and death rates of 22.2 and 22.2%, respectively. Among the patients in groups A2 and B, there was no death or permanent morbidity. Mortality and death rates related to the procedure were 11.1 and 11.1%, respectively for group A, 0 and 0% for group B, respectively. None of the 6 patients with
Poor preoperative grade had excellent results (GOS with score 5) or good (GOS with score 4).
The study also showed that the direction in which the fundus is projected and the subarachnoid hemorrhage appear significantly as risk factors for the micro-surgically treated groups. Improvement in overall surgical outcome includes early surgical intervention for patients with good grade, while subjects with poor grade should be actively managed and evaluated more closely with early surgery.
Endoscopic anatomy of the sella turcica
ABSTRACT
Endonasal endoscopic surgery is a team surgery according to Snyderman et al., which requires learning of non-familiar surgical anatomy, use of new technologies and the development of new surgical skills. The major concerns during surgery are the identification of the internal carotid artery, optic nerves and preservation of small cerebral vessels. The potential for a disaster is great if the surgeon is unfamiliar with the anatomy, there is a lack of adequate equipment and clumsiness to maintain adequate visibility with the endoscope. Many publications speak on the subject, both on transsphenoidal endoscopic anatomy, and on anatomy with the approach by extending its limits.
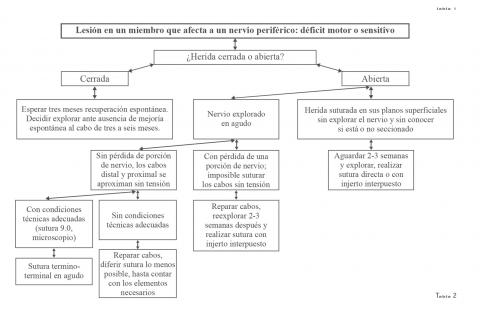
Current concepts in peripheral nerve surgery: When to operate an injured nerve?
ABSTRACT
Peripheral nerve injuries represent a functional deficit of the affected limb that can be reversed if treated properly. The time at which an injury is operated, coupled with the use of the careful microsurgical reconstruction technique, are the most important factors in the final treatment outcome. Open lesions with nerve involvement should be considered surgical in the short term. Closed lesions usually, with the exception of two exceptions described in the text, are scanned from three months to six months after trauma.
It is a frequent occurrence in practice to observe injuries that have lost their ideal repair time, which leads to permanent sequelae. It is important to note that these delays are not seen in the neurosurgical community, but in other specialties that "disbelieve" the usefulness of rapid repairs, or consider that a neurorrhaphy can be performed without adequate instrumentation or magnification. It is to be hoped that in the future every traumatically injured nerve will be rapidly referred to those who are accustomed to the treatment of this type of injury. This will undoubtedly result in better functional outcomes in patients suffering from these lesions.
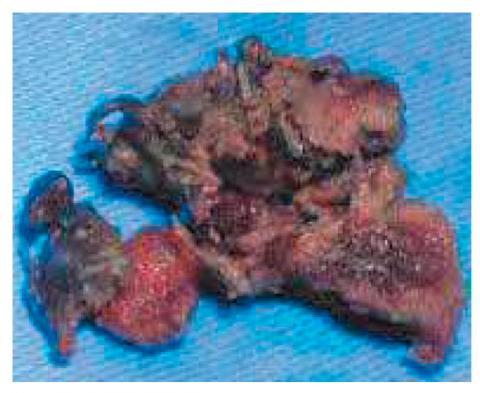
Spinal Cysticercosis: Case Report
ABSTRACT
Cysticercosis is the most common parasitic infection affecting the central nervous system and typically involves the cerebral parenchyma, the subarachnoid space, or the ventricular system. Spinal cysticercosis is rare (0.7-3.2%) even in endemic regions and may require more aggressive management due to the natural confines of the spinal canal. The condition of the lesion, its size, and the inflammatory response generated by cyst degeneration are important factors for the management of spinal CC. We report two cases of spinal cysticercosis in which patients underwent surgical treatment.
Clinical radiological results of segmented instrumentation in thoracolumbar vertebral fractures at Guillermo Almenara National Hospital
ABSTRACT
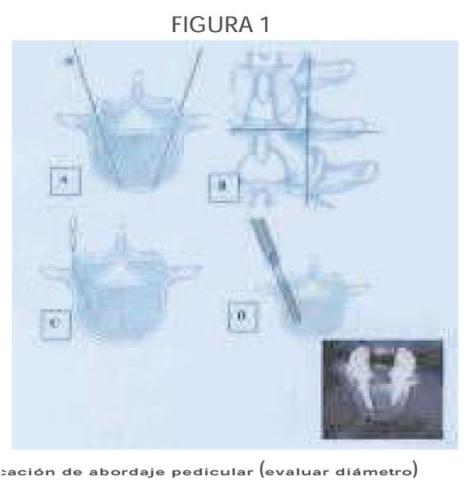
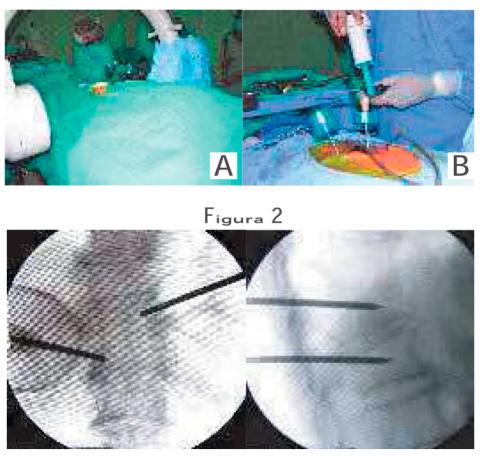
Vertebroplasty in pathological fractures of the spine
ABSTRACT
With the advances in the medicine, we have a high average of life and at the present time leave increment of patient with spine pain for pathological fractures taken place by osteoporosis or in other conditions such as: Spinal metastases, multiple myeloma lesions, and hemangiomas. It is necessary the vertebral stabilization in these patients to improve the pain and at the moment with technical Percutaneous Spinal Vertebroplasty can be reinforced and to give bigger consistency or hardness to the fractured spine.The technique consists to guide placement of the needle and the plastic bone cement that is injected into the vertebrae to stabilize them using Poly methyl methacrylate (PMMA), which is radiopaque due to sterile barium powder, is injected into the bone in the vertebral fractured body, through a stem.Sometimes at level of the spinal compression fractures, we can to introduce and inflates a small balloon into the vertebra to expand its height before injecting the PMMA. This technique is known as Kyphoplasty or Vertebroplasty mediating balloon. The indications of the Vertebroplasty and Kyphoplasty at the moment are the reinforcement of vertebral fractures for spinal metastases too.
In this paper we review the technical basis of the vertebroplasty, according to our experience in this treatment and we present our experience with a small number of cases which had a good outcome for the majority of them.
Arteriovenous malformations in children
ABSTRACT
In cerebral vascular pathology in children, arteriovenous malformations (AVMs) are the most frequent and they are being detected more and more by the technological neuroradiological advances. This has allowed a large percentage to be diagnosed even at the asymptomatic stage. On the other hand, we know that the surgery of these lesions is the fundamental choice as treatment; However in the last decades the Endovascular techniques and radiosurgery have evolved, and currently for the treatment of AVMs, several options are considered as unique or adjuvant according to guidelines established in various hospitals.
With the bibliographical review and personal contribution we want to provide updated information related to epidemiology, clinical picture, diagnosis, treatment and prognosis; And that I hope will help to improve our attention in the neurosurgical patients suffering from this vascular pathology with a often devastating and crippling evolution.