Usted está aquí
Peruvian Journal of Neurosurgery
Radiosurgery in the treatment of brain metastases
ABSTRACT
Radiosurgery may be chosen for brain metastases smaller than 3.5 cm. Of large diameter and with the primary tumor controlled in the following scenarios: 1) Solitary metastases and in good neurological conditions could be treated with radiosurgery only 2) Relatively radioresistant metastases such as melanoma and renal cell carcinoma, 3) Multiple metastases, complementing with total brain radiotherapy, 4) Recurrent metastases. The relative indications for radiosurgery alone, radiosurgery, more radiotherapy, radiotherapy alone and surgical resection remain controversial. Because of its proven efficacy and low morbidity, radiosurgery could be indicated for most cases of brain metastases excluding lesions larger than 3.5 cm, numerous metastases (depending on cumulative volume and whole dose to the brain) and / or with symptomatic mass effect, or causing hydrocephalus. In the latter case the surgery would be the first therapeutic consideration and when a biopsy is necessary to confirm a neoplasia.
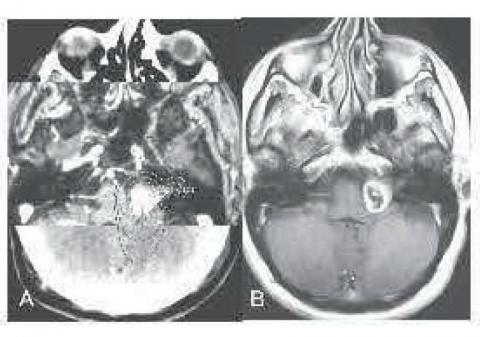
Transcranial doppler to detect regional cerebral vasospasm in patients with SAH of aneurysmal cause.
ABSTRACT
Transcranial Doppler (TCD) is a useful tool in the diagnosis of both regional and diffuse vasospasm, as it is demonstrated in this case (corroborated by angiography). This makes it possible not to reduce triple therapy H when the patient still requires it, TCD is a important arsenal we have, it is not enough clinical diagnosis, since the TCD is noninvasive, fast, online, is performed in bed Patient, and the Doppler vasospasm occurs before clinical vaospasm which makes it a very useful tool. I believe that we are advancing in this area of neuromonitoring in Peru, having as final result patient with favorable evolution, if not for the measurements made.
Pituitary carcinoma: Case report
ABSTRACT
Anaplastic ependymoma in pediatric population
ABSTRACT
History of the Discovery of Normal Pressure Hydrocephalus
ABSTRACT
When we read or hear Normal Pressure Hydrocephalus or chronic hydrocephalus of the adult as it is called at the moment, the Hakim Adams Syndrome comes to our mind immediately. We find it very important to expose the history of the discovery of hydrocephalus at normal pressure,
Pathology that to date has many questions and is a subject of constant research.
Radiosurgery in acoustic neurinoma: Preliminary results at the Pacific Radiosurgery Institute
ABSTRACT
The series of acoustic neurinoma cases treated with LINAC are limited compared to GK. Friedman et al. treated 390 patients. Actuarial control rates at 1 and 2 years were both 98% and 5% at 90%. Only 4 patients (1%) required surgery for tumor growth. Seventeen patients (4.4%) experienced facial paresis and 14 patients (3.6%) reported facial hypoesthesia. The risk of these complications is directly related to tumor volume and / or the prescribed dose at the periphery of the tumor. Since the doses were reduced to 1250 cGy in 1994, only 2 patients (0.7%) had facial paresis and another 2 (0.7%) facial numbness. The safety and efficacy of ER as an alternative to microsurgery in acoustic neurinoma is emphasized.
Cognitive Impairment of Cortical Cognitive Superior Functions in Brain Trauma
ABSTRACT
The presence of neuropsychological alterations in the mental status of patients with brain traumatic injury (BTI). Are characteristic of the disease and are considered as focal symptoms or isolated deficits. In frequency in the BTI. There is a usual way of presenting cognitive impairment. The alterations of the prefrontal cortex and the irregularities of the superior order of the behavior are one of the first psychopathological manifestations of BTI. From the neuropsychological point of view, frontal lobe functions, given their high level of cortical integration and control of other cognitive functions, are difficult to evaluate directly. Some of the earliest evidence comes from the well-known case of Phineas Gage (Harlow 1848-1868), who survived the accident he suffered living until he was 38 years old with the iron rod that pierced the front of his brain and went through the Head, had no obvious neurological deficits, no sensory or motor loss, and was able to speak coherently even after the accident. As the acute effects of the injury diminished, his behavior changed completely, he showed irresponsible, disorderly. The regulation of his behavior was affected by his accident.
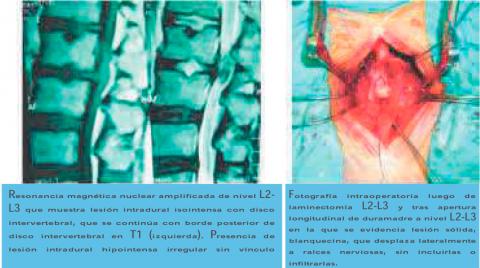
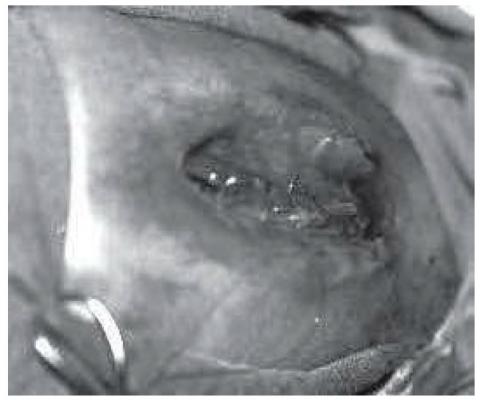
Intradural lumbar disc herniation
ABSTRACT
The disc herniation is one of the most frequent pathologies in the neurosurgical practice. Localization of a portion or all of it in the intradural space is an uncommon complication that can be difficult to differentiate clinically and imagingly from both common hernias and intradural tumors. Its diagnosis is often presumptive until the moment of the surgical treatment. A clinical case of intradural lumbar disc herniation at the L2-L3 level is presented and a review of the pathogenesis, clinical features, imaging findings, treatment and prognosis of these lesions is performed.
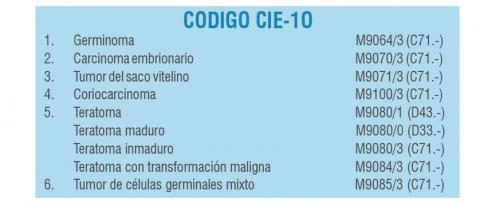
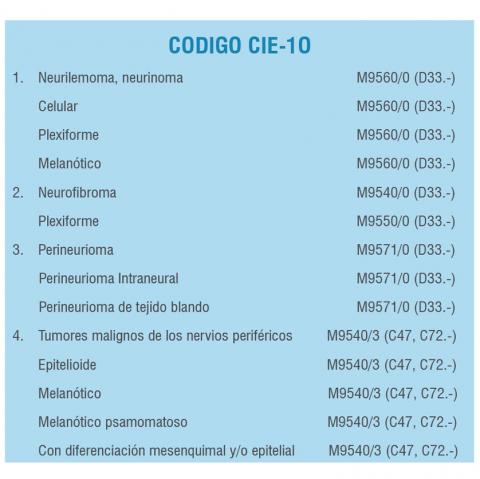
Clinical practice guide of Brain tumours: Part III
ABSTRACT
Tumors of the meninges are primary tumors that originate in meningothelial cells or non-meningothelial mesenchymal cells. The different types of existing tumors are determined by the appearance of the neoplastic cells in the microscope. 2.- Etiology: Unknown. 3.- Pathophysiology: The presence of the tumor in the intracranial level produces an imbalance of the compartments of the intracranial content, that is of the blood volume and the CSF, producing endocanean hypertension. The symptoms and signs presented are related to the topography of the lesion.4.- Epidemiology: Tumors of intracranial meninges account for 10% -15% of all primary intracranial tumors. There are no known epidemiological factors.
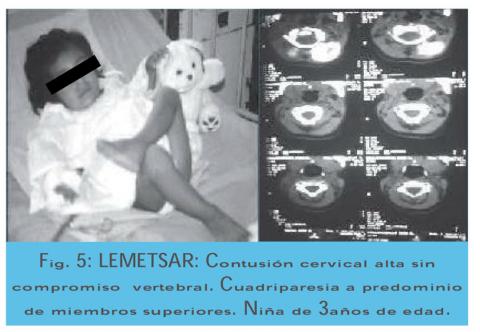
Spine cord injury in children
ABSTRACT
Spinal cord injury is infrequent from infancy to pre-adolescence. The incidence of traumatic lesions of the infantile spinal cord in relation to all age groups oscillates between 0.65% and 11%. Spinal injuries in relation to mild head injuries are 1 / 25-30, and severe head injuries are 1/20; However this incidence may not be as reliable because the statistics are not including minor problems or those that are not hospitalized or survive before reaching the hospital. Cirak et al. have recently studied 406 children under 14 years of age with spinal trauma, with 4% of the total number of patients admitted to the hospital.
The age of 5 to 14 years was predominant in the 36 cases studied. From the study by Cirak et al the average age was 9 years. It has been observed a higher incidence of males in a ratio of 2-3: 1 compared to the female sex; This difference is remarkable in10 years old. This is due to the greater concern, carrying out activities that demand greater risk (sports practice, driving motor vehicles, etc.) and drug consumption by older children and adolescents. On the other hand we have observed that these traumatic problems of the rachis and marrow occur mainly in the evenings and nights. Ducker and Perot report that in their cases studied at night and dawn were the predominant moments.
Direct Anterior Fixation with Cannulated Screws in Odontoid Fracture
ABSTRACT
The fractures of Odontoid type II according to the classification of Anderson and D'Alonzo are considered the most unstable and were always difficult to handle. External immobilization is used as a frequent method by some authors, however surgery provides better fixation. Back surgery such as inter laminar and Magerl interfacetaria are used but they block the rotational mobility of the atlas axis segment. Bohler describes the first surgeries previously, this technique was modified in recent years and is currently being performed with minimally invasive approach techniques.
In the present work we present the experience of the technique used in our series and a review of the literature with respect to this pathology and the techniques of management of such lesions.
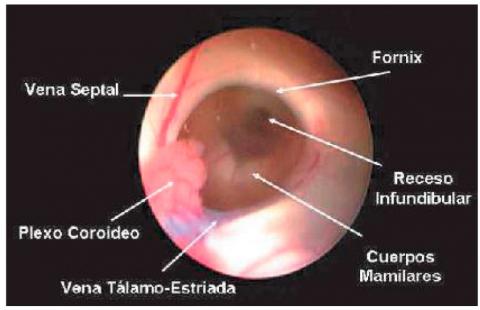
Surgical practice guide of Third Endoscopic Venriculostomy
ABSTRACT
Minimally invasive surgical procedure performed through a single hole in the skull (monoportal), with the use of a neuroendoscope to allow the fenestration of the floor of the third ventricle, thus communicating the ventricular system with the subarachnoid space.
The third endoscopic ventriculostomy indications are: Obstructive or Non-Communicating Hydrocephalus (as the main indication) for: Silvio aqueduct stenosis, Tumor obstruction of cerebrospinal fluid circulation. In other types of hydrocephalus its efficacy is lower.
Clinical practice guide of Brain tumours: Part II
ABSTRACT
In tumors of the posterior fossa and previous analysis of the neurological conditions upon admission (in adults, Karnofski greater than and equal to 70) and the age of the patient, a ventriculoperitoneal shunt will be planned first if there is hydrocephalus or when in Each case is justified; Then total or subtotal or partial resection of the tumor will be performed to decompress the cranial cavity, reduce endocranial hypertension in the posterior fossa, and obtain tumor material for histopathological analysis. If the tumor is located at the intraspinal level, a total or partial resection will be performed, when the patient still retains some degree of motor function in the limbs; However if there is paraplegia or quadriplegia complete grade 0/5 long installation, the operation would not be justified since it is known beforehand that motor-sensory-sphincter function will not recover. The next form of complementary treatment could be with radiotherapy for some cases with residual tumor and according to the pathology.
Epidemiology of traumatic brain injury in children
ABSTRACT
Surgical practice guide of Myelomeningocele in emergency
ABSTRACT
Myelomeningocele is the most frequent and complex congenital malformation that is compatible with life. Our institution as a reference center at the national level for pediatric neurosurgical pathology receives with relative frequency transfers of infants with open spina bifida. According to the Office of Institutional Statistics and Informatics in Peru, during 2006, congenital malformations were the main cause of hospitalization in the neurosurgery service, with myelomeningocele being the second cause after congenital hydrocephalus.