Usted está aquí
Peruvian Journal of Neurosurgery
Brain abscess: Clinical and therapeutic study in a county hospital in Peru
ABSTRACT
The onset symptoms are: headache in 50%, seizures 17%. The main symptom: convulsions in 66%, hemiparesis and alterations of the sensorium. The clinical picture was characterized by headache (83%), convulsions (66%), hemiparesis (66%), fever (66%), aphasia (50%), papilloedema and vomiting (50%) Meningeal and prefrontal signs (33%). Clinical syndromes: headache (83%), focal neurological (83%), focal (67%), febrile (67%), HEC (50%), meningeal (33% %).
CT scan and cerebral MRI revealed 6 cases of cerebral abscess, of right hemispheric location in 5 cases, 3 single and 3 multiple cases; 2 in the frontal lobe, 1 frontalparietal, 1 frontotemporal and 1 parietal. Two cases in cerebritis and 4 encapsulated phase, with surrounding edema and mass effect. The treatment was done with cefotaxime 1 gr c / 6 hs. VEV / 20 days, or ceftriazone 2 g c / 12 h VEV / 20 days, together metronidazole 500 mg c / 6hs. EV / 20 days. In 1 case the treatment was prolonged up to 60 days with oral metronidazole. The sequelae were: hemiparesis, prefrontal alterations, convulsions, metronidazole peripheral polyneuropathy. The clinical and tomographic evolution was favorable in 4 cases, 2 patients died.
Odontoid fracture type II
ABSTRACT
Odontoid type II fractures are relatively frequent and its therapeutic approach continues to be subject to considerable debate by the different column groups, both national and international. It is a young woman who suffered a traumatic brain injury in a traffic accident although there was no neurological compromise, persistent neck pain led to the diagnosis of a type II odontoid fracture. Faced with refractoriness to conservative treatment the patient was taken to surgery, in which an anterior fixation of the odontoid process was performed.
Odontoid fractures type II can be treated with a surgical or medical approach, each with advantages and disadvantages and in any case none free of morbidity. Surgical treatment is indicated by the failure of the conservative approach.
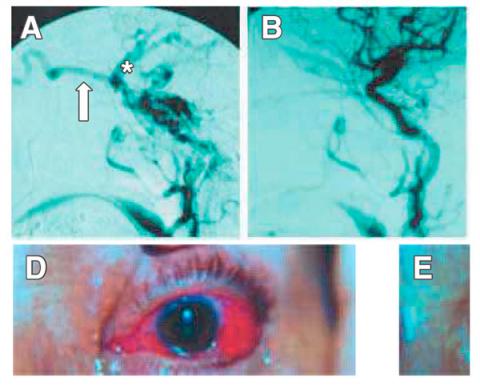
Endovascular Embolization of Cavernous carotid fistulas. Personal experience 1994- 2004
ABSTRACT
Patients and methods: Clinical and radiological data from 21 CCF treated between October 1994 and July 2004 were retrospectively analyzed.
Results.- Of 21 CCF 13 were direct and 8 indirect. The most frequent symptoms were red eye, murmur, exophthalmos and diplopia. Of the 21 CCF treated by endovascular techniques in the present study, 85.71% (18/21) were cured. An additional CCF was obliterated almost completely, constituting 4.76% (1/21). The attempt of embolization by both vascular routes was failed in 2 cases (2/21), 9.52%. Symptomatic complications occurred in a total of 9.52% of the cases (2/21), having a permanent neurological character in 4.76% (1/21) and transient in 4.76% (1/21%). The cured patients in our series improved their symptoms of orbital congestion in a few weeks while the paresis of oculomotors improved slowly or did not change from the preoperative period during the observation period.
Conclusion.- The endovascular embolization of the present series of CCF proved a very effective and safe treatment, managing to cure or improve in a significant and permanent way a vast majority of patients with results comparable to those reported in the international reference centers.
Endoscopic endonasal approach of Pituitary macroadenoma. First experience in Peru 2008
ABSTRACT
Management of multiple intracranial aneurysms
ABSTRACT
Multiple intracranial aneurysms (AIM) are relatively common, occurring in approximately 23% of all patients with aneurysms. The risk factors include female gender, hypertension, smoking and family history possibly intracranial aneurysms or cerebrovascular disease. The ruptured aneurysm location can be determined with a high accuracy rate with digital angiography when used in conjunction with computed tomography (CT) and magnetic resonance (MR). The average breakdown of untreated multiple aneurysms is between 1 and 2.2%. The critical size associated with significant risk of bleeding was 7 mm. Multiple aneurysms occur most often along the internal carotid artery (ICA) and the bifurcation of the middle cerebral artery (MCA). After bleeding is of any of the aneurysms, you must diagnose what was it bled, and which should be the first to be clipped, this is important especially when all aneurysms can not be clipped with a single approach. Most multiple intracranial aneurysms of the anterior circulation can be clipped by fronto-temporo-sphenoid approach; inclusive aneurysms on the contralateral side.Also, the development of new endovascular techniques (use of hidrocoils, bioactive coils, onyx, remodeling techniques with balloon or stent aneurysm single or double), permit more satisfactory treatments, including combining both techniques.
Conclusion: Multimodal approaches combining microsurgical and endovascular treatment, have been used successfully in cases of multiple cerebral aneurysms.
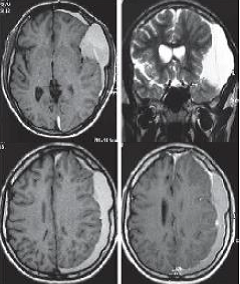
Chronic Subdural Hematoma in young patient: Complicated congenital Arachnoid Cyst
ABSTRACT
Chronic subdural hematoma (CSDH) is a common pathology in daily neurosurgical practice that usually develops in older people due to brain atrophy related to age, being rare in young people. We report the case of a patient of 16 years with a HSDC formed a left temporal congenital arachnoid cyst, which
simulated a meningioma plane, which was operated by craniotomy and resection of membranes, and its postoperative course was favorable Young people may also have HSDC if they have similar conditions that favor developmentof chronic subdural hematoma in the elderly, such as a congenital arachnoid cyst, which is a major risk factor for chronic hematoma in young and should be considered in the differential diagnosis of these lesions. Surgical treatment may be performed by trephination and irrigation or by craniotomy.
Stereotactic Radiosurgery in Neurinomas and Meningiomas of Skull Base
ABSTRACT
We report our experience with LINAC stereotactic radiosurgery for tumors of the skull base: 32 patients (21 meningiomas and 11 acoustic neurinomas) tracked over 20 months between November 2004 and July 2010. 17 received before radiosurgery, surgical treatment with partial tumor resection. With a median of 32 months after radiosurgery, tumor control is evident in 97% of cases, including 10 cases had tumor regression and tumor necrosis 12, making 22 cases with frank tumor regression. 9 patients remain under observation with no change in tumor size but incipient necrosis. A patient with acoustic neuroma showed tumor growth at 36 months of observation for which he received a second treatment with radiosurgery. Among the functional effects of radiosurgery., 9 of the 10 patients with trigeminal neuralgia were recovered, 2 of 3 cases with oculomotor nerve paresis and 1 patient with ptosis recovered normal ocular motility. A patient with neurofibromatosis 2 deaf evolved despite its tumor regression. Benign tumors of the skull base have their personalized treatment option, either as primary therapy after subtotal resection or recurrence, radiosurgery is the best choice because it provides high rates of regression with control or low risk of complications.
Percutaneous microcompression of the Gasser ganglion for trigeminal neuralgia. Clinic Maison de Santé 2005 – 2009
ABSTRACT
Objective: Demonstrate the effectiveness of the percutaneous microcompression of the Gasserian ganglion with the balloon of Fogarty in the surgical treatment of trigeminal neuralgia.
Patients and methods: There was realized a descriptive retrospective and prospective study of 24 patients with trigeminal neuralgia treated surgically by the technique of percutaneous microcompression of the Gasserian ganglion with the balloon of Fogarty in the Clinics Maison de Santé between January 2005 until December 2009. The medical records and operative reports were review and the data were grouped according to study variables.
Results: The 66.7% of patients were female. The mean ages for the patients were 63.1 +/- 11.9 years and the average time of the disease was 8.1 +/- 4.8 years. The right side of the face was the most affected in 70.8%, and the trigeminal branches most affected were the combination of the second and third at 50%. The mean operating time was less than 30 minutes. In 91.7% of patients had no facial pain after surgery and no recurrence at one year by 83.3%.
Conclusions: The percutaneous microcompression of the Gasserian ganglion with the balloon of Fogarty is a highly effective technique in the surgical treatment in patients with trigeminal neuralgia.
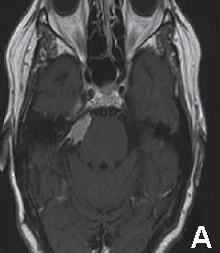
Trigeminal Neuralgia by cerebellopontine angle epidermoid cyst
ABSTRACT
Trigeminal neuralgia is classically described as one of the most severe facial pain syndromes. Usually it is defined as a paroxysmal, lancinating, electric-type pain, recurrent and usually unilateral, in the distribution of one or more divisions of the trigeminal nerve. Typical trigeminal pain is characterized by intermittent, generally with periods of exacerbation and remission. The annual incidence of this pathology varies between 4 and 13 per 100, 000 individuals. The male:female ratio is 1:1.5. Although cause of trigeminal neuralgia is idiopatic, exist cases associated to compression of the trigeminal nerve by a vascular structure or tumors. Epidermoid cysts are tumors of embryological origin that are located in cerebellopontine angle in third place after schwannomas and meningiomas. Three cases of trigeminal neuralgia in relation to epidermoid cysts of the cerebellopontine angle compressing the trigeminal
nerve are presented. Clinical presentation, diagnostic studies, surgical treatment and postoperative results are discussed.
Key words: Trigeminal neuralgia, trigeminal nerve, epidermoid cyst, neuropathic pain, cerebellopontineangle.
Awake Craniotomy for resection of low grade glioma. First experience in Perú 2008
ABSTRACT
The aim of the brain tumour surgery is the maximal tumour resection with the minor neurological post operatory deficit; nevertheless this is not always possible mainly in case of lesions near to functional areas. Despite the use of numerous technologies of images before and during and during the operative period, the functional result is unknown but after the surgery when the deficit is irreversible. The awake craniotomy is a safe technique and that it allows to evaluate the neurological status during the surgical act and to detect prematurely any deficit in the function, which allow us optimize the results of the tumour resection. We presented the first report of case in Peru of awake craniotomy for low grade glioma resection, carried out in the Guillermo Almenara National Hospital in February 2008.
Key Words: Awake Craniotomy, surgery, low grade astrocytoma
Technique of the “cono embossed or cone of cookie” on the reconstruction of the neck at displastic giant aneurysm of the carotide paraoftalmic siphon: Intra-aneurismal Stent
ABSTRACT
The dysplastic giant aneurysm with wide neck is a difficult complex aneurysm surgery, the use of endovascular therapy in this pathology is promising and waffle cone technique is very useful in those in wich when we use a Stent and it is impossible to exceed the distal end of the aneurysm neck. A woman patient of 73y, housewife with disease duration of 5 days, headache associated with neck stiffness and cranial nerve VI paresis of the left was studied. The brain CT showed subarachnoid hemorrhage in the left sylvian valley and an image suggestive of a giant aneurysm of left carotid siphon. The angiographic study concluded giant-ophthalmic aneurysm ruptured left and right paraoftálmic large aneurysm not broken.
The treatment of choice for aneurismal disease is still under discussion, but in the case of giant aneurysm endovascular techniques may achieve optimal results without major complications, endovascular technique waffle cone through the use of Stents is very useful and should extend its use in those dysplastic giant aneurysm with wide neck do not allow the stent to achieve beyond the distal aneurismal neck and both nest in the pouch is able to embed a Neuroform Stent-in the neck of the aneurysm to proceed to use coils of different dimensions to completely embolize the aneurysm. The disadvantages of this technique are the potential for drilling and higher rate of recanalization caused by changes in arterial blood flow. Waffle cone technique is particularly useful in those dysplastic giant aneurysms with wide neck in wich the structure of the aneurysm does not allow the location of the stent at the distal end of its neck.
Subarachnoid hemorrhage II: Cerebral aneurysms
ABSTRACT
Subarachnoid hemorrhage (SAH) is defined as the presence of blood in the subarachnoid space and cisterns of the base. The source is variable and may be due to rupture of intracranial aneurysms (80%), arteriovenous malformations (AVMs), tumors and trauma cranoencefálicos. The HSA is a relatively common disease with an incidence is 5% of cerebral vascular disease. The estimated prevalence of 10 new cases per 100,000 people each year. The proportion of HSA varies with age, being the most prevalent group between 50 and 60. It is a pathology with high morbidity and mortality, since a high percentage of patients (10-15%) did not reach the hospital and the remaining group of about 15% die. Angiography is the standard diagnostic procedure, although angiography is an important alternative. Treatment should be administered as soon as possible within 72 hours, both surgical and endovascular techniques to prevent complications such as rebleeding, vasospasm and hydrocephalus, being the most widely used surgical approach is the pterional craniotomy. The prognosis depends on careful handling and the degree of the initial hemorrhage.
Key words: Subarachnoid hemorrhage, Intracraneal aneurysm, Craniotomy.
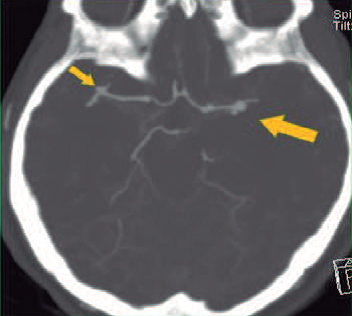
Subarachnoid hemorrhage I: Diagnosis and Management
ABSTRACT
Subarachnoid hemorrhage (SAH) is defined as the presence of blood in the subarachnoid space and cisterns of the base. The source is variable and may be due to rupture of intracranial aneurysms (80%), arteriovenous malformations (AVMs), tumors and trauma cranoencefálicos. The HSA is a relatively common disease with an incidence is 5% of cerebral vascular disease. The estimated prevalence of 10 new cases per 100,000 people each year. The proportion of HSA varies with age, being the most prevalent group between 50 and 60. It is a pathology with high morbidity and mortality, since a high percentage of patients (10-15%) did not reach the hospital and the remaining group of about 15% die. Angiography is the standard diagnostic procedure, although angiography is an important alternative. Treatment should be administered as soon as possible within 72 hours, both surgical and endovascular techniques to prevent complications such as rebleeding, vasospasm and hydrocephalus, being the most widely used surgical approach is the pterional craniotomy. The prognosis depends on careful handling and the degree of the initial hemorrhage.
Key words: Subarachnoid hemorrhage, Intracraneal aneurysm, Craniotomy.
Pterional Keyhole Approach for treatment of Aneurysms 2009
ABSTRACT
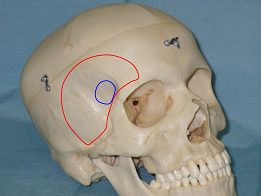
Objective: The pterional approach is the most common approach in vascular neurosurgery, but in recent years has been an increasing interest in minimally invasive surgery or keyhole surgery. We present preliminary results from the use of pterional keyhole approach in surgery for cerebral aneurysms performed in the Cayetano Heredia Hospital in 2009.
Patients and Methods: We performed a pterional keyhole craniotomy of 2.5 x 3 cm from a curved incision of approximately 5-6 cm behind the hairline and centered on the orbitofrontal and posterior aneurysm clipping, in patients with late aneurysms, CoP, bifurcation ICA and MCA aneurysms, Hunt and Hess I-III, without edema, associated vasospasm or hematoma.
Results: From January to December 2009 six patients were operated by pterional keyhole approach, 4 with CoP aneurysms (66%), 1 with ACI (17%) and 1 with ACM (17%). All were operated on late and Hunt and Hess was I in 3 cases (50%) III in 2 cases (33%) and II (17%). There were no operative complications and the outcome was favorable in most cases: Rankin 1 (50%) and Rankin 2 (33%).
Conclusions: The pterional keyhole approach is a minimally invasive surgery for brain aneurysms, which maintains the advantages of the standard pterional approach but it minimizes the exposure of brain parenchyma and soft tissue manipulation. It is a valid surgical alternative in selected cases, mainly from CoP and MCA aneurysms.
Key Words: Pterional approach, craniotomy, aneurysms, minimally invasive.
Two years of Lumbo-sacral spine dynamic stabilization in Rebagliati-Essalud Hospital during the period January 2012-October 2013
ABSTRACT
Objective: To determine the clinical outcome in patients undergoing dynamic stabilization in the neurosurgery spine service at HNERM during the period January 2012 to October 2013.
Methods: 25 patients with unstable spine that met the inclusion criteria for the placement of dynamic spine stabilization were selected.
Results: The average age of patients 46.4 years, minimum 6 and maximum 78 years. Sex: Male 16 (64%) Female 09 (36%) total 25 (100%). No previous lumbar 23 (92%), discectomy 02 (08%): prior lumbar surgery Sick time (months) 25.8 average, minimum 3 and maximum 72. Surgical approach Wiltse Total 15 (60%), medial approach 9 (36%) type, Hoober 1 (4%) 25 Instrumentation levels; 2 level 4 (16%), three levels 21 (84%). Days in hospital: average 3.72 min 3 max 5. Preoperative clinical features: EVA average 7.92 min 6 max 10 mod 8. Pain intensity mod 13 (52%), severe12 (48%). Postoperative clinical features: EVA average 4.16 min 3 max 8 fashion: 3. Pain intensity: mild 19 (76%), moderate 05 (20%) and severe 04 (14%).
Conclusions: Dynamic stabilization has demonstrated efficacy in pain control with a minimum length of hospitalization.