Spontaneous intraventricular pneumocephalus associated with transient aphasia: case report and review of the literature
ZINDYA BARRRIENTOS M., CAMILO CONTRERAS C.
Abstract (Spanish) ||
Full Text ||
PDF (Spanish)
ABSTRACT
Introduction: Pneumocephalus or the presence of air in the cranial cavity is common after a craniotomy and in patients with traumatic brain injury; however, its spontaneous appearance is extremely rare. So far, very few cases of spontaneous intraventricular pneumocephalus have been reported. We present the case of a patient who developed spontaneous intraventricular pneumocephalus, which required a craniotomy for surgical correction.
Clinical Case: A 59-year-old female patient with a history of left suboccipital craniotomy and resection of the left vestibular Schwannoma who after 2 years presented headache of 3 weeks duration and aphasia of expression. On examination: Mild expressive aphasia, surgical scar with no evidence of cerebrospinal fluid (CSF) leakage. Brain tomography (CT) showed pneumoventricle in the frontal and temporal horns of the left lateral ventricle and deviation from the midline; radionuclide cisternography was negative for CSF fistula and CSF analysis was normal. A left subtemporal craniotomy was performed, finding a bone defect in the petrous portion of the temporal bone above the internal auditory canal associated with a meningocele of the medial base of the skull, which was sealed with bone wax, fat, fascia lata, and biological glue.
Conclusion: The first case of spontaneous intraventricular pneumocephalus without identifiable CSF fistula is described, which made this case extremely rare. The treatment performed was a surgical correction of the meningocele through a subtemporal extradural approach, and the patient presented a favorable evolution with the improvement of the aphasia.
Keywords: Pneumocephalus, Aphasia, Meningocele, Craniotomy, Temporal Bone (source: MeSH NLM)
High-definition three-dimensional exoscopy-guided exeresis of a ruptured supratentorial cavernous angioma. Initial experience at the Dos de Mayo National Hospital.
JOSÉ LUIS ACHA S., LUIS CONTRERAS, MIGUEL AZURÍN, MANUEL CUEVA, ADRIANA BELLIDO; SHAMIR CONTRERAS
Abstract (Spanish) ||
Full Text ||
PDF (Spanish)
ABSTRACT
Introduction: We report the exeresis of a cerebral cavernoma, by using the extracorporeal telescope ("exoscope") operating system integrated into the Kinevo 900 microscope. The objective of this study was to evaluate the surgical potential of this novel high-speed 3D exoscope system. definition (4K-HD) for the removal of a brain cavernoma.
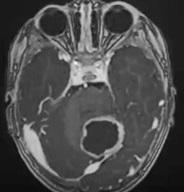
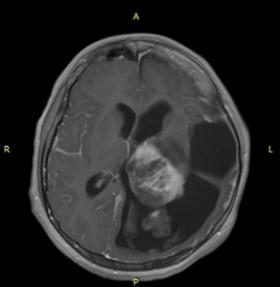
Clinical Case: A 47-year-old female patient was admitted to the emergency room for having presented intense headache with occipital predominance, the tomography showed a right occipital hematoma, the presence of a ruptured cerebral cavernoma was confirmed, so surgery was decided. The exoscope allowed good maneuverability of the instruments, without visual obstruction. The large 4K monitor made for an immersive surgical experience, giving multiple team members the same high-quality 3D view as the primary operator. It was also ergonomically favorable, allowing the surgeon to be in a neutral position regardless of the operative angle.
Conclusion: The novel system provided excellent visualization, ergonomics, and favorable maneuverability, the shared surgical vision of the exoscope with 3D lenses provided educational advantages for our residents. More cases are justified to validate this initial experience.
Keywords: Hemangioma, Cavernous, Central Nervous System, Telescopes, Ergonomics, Brain. (Source: MeSH NLM
Giant occipital encephalocele in a newborn; surgical treatment. Case report
GABRIELA ESPIN O., ALICIA TORRES M., JOSE RODOLFO BERNAL C., JESUS CASTRO V., ANDREA PAEZ C., BYRON SANUNGA V., CARLOS MORALES T., ENRIQUE CASTRO S.
Abstract (Spanish) ||
Full Text ||
PDF (Spanish)
ABSTRACT
Introduction: Neural tube defects (NTD) are congenital malformations that are caused by the lack of fusion of the neural tube during the embryonic period, exposing the nervous tissue to the outside. There are different types, and they can be cranial (anencephaly and encephalocele) and spinal (spina bifida). The encephalocele is a protrusion or herniation of the intracranial content, through the bony defect of the skull. In this article, we report the case of a patient diagnosed with occipital encephalocele, while reviewing the neurosurgical treatment performed in our hospital.
Clinical Case: We present the case of an 8-day-old male neonate, the son of a 36-year-old diabetic mother, with a prenatal ultrasound diagnosis of occipital encephalocele, evidenced at 16 weeks of gestational age. The patient underwent surgery, performing a plasty of the occipital encephalocele; he presented as a mediate complication infection of the surgical wound that was resolved with antibiotic treatment, later presenting a favorable evolution.
Conclusion: The extension and nature of the hernial content of the encephalocele determine its prognosis, as well as immediate treatment, which can reduce postoperative complications.
Keywords: Encephalocele, Neural Tube, Spinal Dysraphism, Nerve Tissue (Source: MeSH NLM)
Articulated robotic arm for assistance in interventional radiology
ROLANDO ORTEGA, IVAN ORTEGA, DEISY ACOSTA, JORGE POMA, LUZ CASTAÑEDA
Abstract (Spanish) ||
Full Text ||
PDF (Spanish)
ABSTRACT
|
Objectives: Robotic technology has helped medicine to reduce exposure time and offer greater efficiency and precision in surgical interventions. The goal of using an articulated robotic arm for X-ray (Rx) guided minimally invasive surgery and interventional assistance is to reduce direct and secondary radiation on physicians. The use of a collaborative robotic arm (COBOT) that replaces the operating arm of the surgeon-interventionist physician to avoid exposure to X-rays is described.
Methods: The COBOT has a remote-controlled electronic gripper and includes a special needle holder made using 3D printing technology; This holds the interventional instrument, needles, and other surgical elements. The instrument-loaded forceps are oriented and progressed toward intracorporeal therapeutic target points used in interventional radiology and radiation therapy procedures, the COBOT boasts operational precision.
Results: Its operation was verified by simulating the interventional action in models in animal tissue, and experimental surgery laboratory.
Conclusions: It is concluded that the robot arm can perform assistance functions in radiological and stereotaxic neuroradiological interventionism with a good level of precision, reducing the doctor's exposure to X-rays.
Keywords: Robotics, X-Rays, Radiology, Interventional, Robotic Surgical Procedures (Source: MeSH NLM)
|
Nosocomial infections in neurosurgery: a study of incidence, associated factors and etiology. Cayetano Heredia Hospital. April 2020 - March 2021
ELDER CASTRO C., ROMULO RODRIGUEZ C.
Abstract (Spanish) ||
Full Text ||
PDF (Spanish)
ABSTRACT
Objectives: To determine the incidence, associated factors, and etiology of nosocomial infections (NI) in patients hospitalized in a neurosurgery service.
Methods: Descriptive, retrospective, and cross-sectional study in patients 18 years of age and older, hospitalized in the Neurosurgery Service of Hospital Cayetano Heredia (HCH), between April 2020 and March 2021. Data were collected from medical records, registry care diary, and the HCH laboratory computer system.
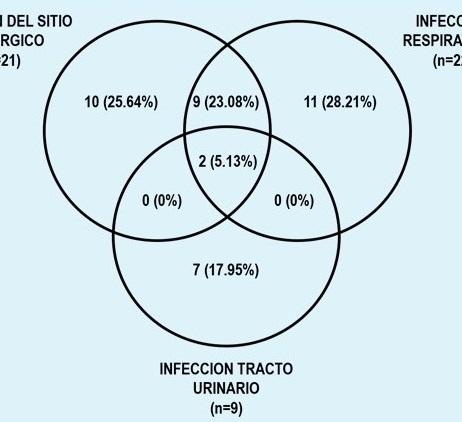
Results: Of the total number of patients (n=116), the male sex (73.28%) and the age between 18 to 59 years (73.28%) predominated. 35.34% had at least one NI, being the most common pneumonia (18.97%) and surgical site infections (SSI) 18.10%. NI were associated with traumatic brain injury (TBI) (p=0.005), spinal cord trauma (SCI) (p=0.020), surgery (p=0.032), stay in Intensive Care Units (ICU) (p=0.000), hospital stay greater than seven days (p=0.000) and mortality (p=0.049). Pneumonia was associated with all the above factors, except trauma and surgery; while SSIs were associated with these factors except for SCI, the performance of surgery, and mortality. Gram-negative agents and enterobacteria were the most frequent in SSIs (72.73%) and pneumonia (94.74%).
Conclusions: NIs occurred in a third of the patients; increasing in those with traumatic pathology, undergoing surgery, admitted to the ICU, and prolonged hospital stay; thereby increasing mortality. It is unavoidable to consider the presence of Gram-negatives and enterobacteria when using antimicrobials in the treatment of NI in neurosurgical patients.
Keywords: Pneumonia, Surgical Wound Infection, Neurosurgery, Brain Injuries, Traumatic (Source: MeSH NLM)
Intracerebral hemorrhage of basal ganglia, surgical management through transinsular transylvian approach. case report
GIUSEPPE ROJAS P.1a, JESÚS FLORES Q.2b
Abstract (Spanish) ||
Full Text ||
PDF (Spanish)
ABSTRACT
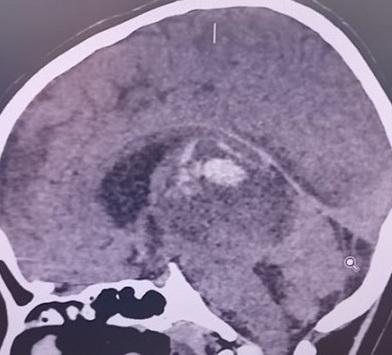
Introduction: Acute spontaneous intracerebral hemorrhage is a life-threatening disease of global importance, with a poor prognosis and few effective treatments. For supratentorial intracerebral hemorrhage, early evacuation (<24 hours after hemorrhage onset) with standard craniotomy is considered lifesaving in deteriorating patients. In cases where the hemorrhage is less than 1 cm from the cortical surface, the clinical benefit is even greater.
Clinical case: We present the case of a 56-year-old obese male patient with a history of high blood pressure who was admitted with an extensive intracerebral hematoma in the basal ganglia of the right hemisphere. A right frontoparietotemporal craniotomy was performed, with the opening of the Sylvian fissure and approach through the insula, managing to evacuate the hematoma. The initial evolution was stationary, so it was necessary to remove the bone platelet, thereby achieving a favorable evolution, then performing the cranioplasty.
Conclusion: Surgical treatment of intracerebral hemorrhage of the basal ganglia through the transylvian transinsular approach has shown good results in several case series in terms of evacuation degree and functional outcome. In addition, this approach spares the frontal and temporal cortex, sometimes avoiding a decompressive craniectomy and its complications
Keywords: Cerebral Hemorrhage, Hematoma, Decompressive Craniectomy, Basal Ganglia (source: MeSH NLM)
Venous sinus thrombosis secondary to severe traumatic brain injury. case report
MARCOS VILCA A., MARCO MELGAREJO P., ERMITAÑO BAUTISTA C., CARLOS PALACIOS P., YURIKO VILLAREAL H.
Abstract (Spanish) ||
Full Text ||
PDF (Spanish)
ABSTRACT
Introduction: Cerebral venous thrombosis (CVT) is a rare type of cerebrovascular disease that can occur at any age and represents 0.5% to 1.5% of the total.1 Superior sagittal venous sinus thrombosis (SSVST) secondary to brain injury (BTI) is reported worldwide only as single cases or in small series.3,4 Headache is the most frequent symptom (90%). The most common focal signs are aphasia and hemiparesis. Papilledema occurs in 25% of cases and epilepsy in about 40%.1,4 Diagnosis is made by venous phase angiography, or by magnetic resonance imaging (MRI) with gadolinium or computed tomography (CT)1,2.
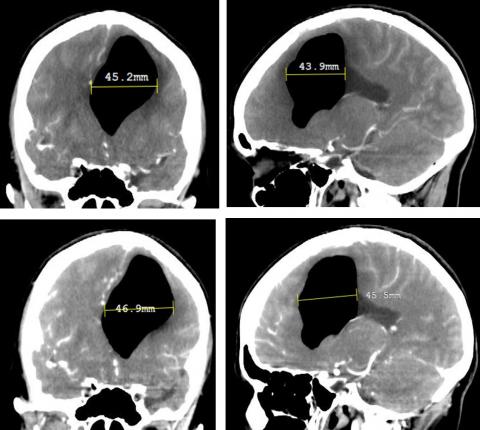
Clinical Case: 23-year-old woman who suffers a traffic accident as a passenger. He presented explosive vomiting, loss of consciousness and seizures, brain CT showed multiple bifrontal contusions, midline deviation> 5mm, cisternae of the base obstructed, Glasgow Coma Scale of 6. A decompressive craniectomy was performed and then he was transferred to ICU for management of intracranial hypertension. She presented with hydrocephalus, nervous system infection (ventriculitis) and superior sagittal venous sinus thrombosis.
Conclusion: SSVST post BTI is a rare cause of SSVST, but potentially dangerous if not diagnosed early. The magnitude of the trauma does not correlate with the appearance of VST. The most common symptom is headache, followed by seizures and signs of targeting, which correlate with lesions in the brain parenchyma.
Keywords: Sinus Thrombosis, Intracranial, Intracranial Hypertension, Brain Injuries (Source: MeSH NLM)
Intracerebral foreign body granuloma simulates a brain tumor. case report
JOHN VARGAS U., MANUEL LAZÓN A., MARCO MEJÍA T., JOHN MALCA B., FERNANDO PALACIOS S.
Abstract (Spanish) ||
Full Text ||
PDF (Spanish)
ABSTRACT
Introduction: An intracranial foreign body granuloma is a chronic inflammatory reaction, due to materials used in cranial surgery; this complication is rarely reported in neurosurgery. The definitive diagnosis is by pathological anatomy since the images are very similar to those of a brain tumor. Treatment is total resection of the lesion.
Clinical Case: A 2-year-old female patient, with a history of surgery for ventricular shunt and exeresis of a pilocytic astrocytoma, with contrast imaging study 6 months after surgery where a lesion suggestive of tumor recurrence was observed, for which she received chemotherapy with vincristine and carboplatin, without positive response. The patient presented to the examination, an extension of the base of support, Glasgow Coma Scale (GCS): 15 points. She underwent surgery, achieving total resection of the lesion. The final diagnosis was intracranial foreign body granuloma. The evolution was favorable, without neurological sequelae or residual tumor.
Conclusion: Intracranial foreign body reaction is a rare pathology but should be considered in the differential diagnosis of disease progression in neuro-oncology patients.
Keywords: Granuloma, Foreign-Body, Astrocytoma, Neoplasm, Residual, Brain Neoplasms, (source: MeSH NLM)
Fusocellular / pleomorphic sarcoma in a patient with Haberland syndrome
IVAN FLORES, JOHNNY MONTIEL, FAUSTO GUERRERO.
Abstract (Spanish) ||
Full Text ||
PDF (Spanish)
ABSTRACT
Introduction: The first case of pediatric spindle cell / pleomorphic sarcoma associated with Haberland syndrome or Encephalocraniocutaneous Lipomatosis, a rare ectomesodermal dysgenesis defined by the triad that includes ocular, skin, and central nervous system involvement, which is usually unilateral, is described. This disorder is attributed to a postzygotic mutation responsible for dysgenesis of the neural tube and crest.
Clinical Case: We present the case of a 10-year-old boy, who evolves with developmental delay, motor deficit, intellectual deficit, and epilepsy, associated with spindle cell / pleomorphic sarcoma. We describe his clinical evolution, electroencephalography, and neuroimaging of him.
Conclusion: The hypothesis that Haberland syndrome is associated with an increased risk of tumor development is intriguing, although the rarity of the disease currently prevents us from drawing definitive conclusions about this possible link between the two entities.
Keywords: Encephalocraniocutaneous lipomatosis, Sarcoma, Epilepsy, Central Nervous System. (Source: MeSH NLM)
Injured glioma syndrome: report of a case with unfavorable outcome
DANILO ZAVALAGA N., ERMITAÑO BAUTISTA C.
Abstract (Spanish) ||
Full Text ||
PDF (Spanish)
ABSTRACT
Introduction: Wounded Glioma Syndrome (WGS) is a clinical picture described after resection of high-grade tumors. It is characterized by the presence of hemorrhage and postoperative edema that is difficult to manage, leading to significant sequelae and in some cases death. Pre and postoperative conditions play an important role in WGS, as well as factors related to surgery such as modification of tumor and peritumoral blood flow, altered coagulation, among others.
Clinical case: 12-year-old patient with a diagnosis of anaplastic astrocytoma who underwent partial surgical resection, without presenting complications. At 48 hours, the patient presented clinical signs of intracranial hypertension, the brain tomography revealed bleeding in the surgical bed and significant perilesional edema. Barbiturate coma, neuroprotective measures, and anti-edema treatment were induced. The patient remained in the ICU for 23 days, leaving the ICU on a 5-point Glasgow Coma Scale, dependent on mechanical ventilation so far.
Conclusion: This case shows the rapid deterioration and important sequelae that a patient with glioma surgery can present. Complete resection is not always possible. Therefore, when faced with incomplete resection or a biopsy, neurosurgeons must consider this syndrome, as well as its implications and repercussions in the immediate postoperative period; To assess the risk/benefit when planning surgery and act early, if this syndrome occurs.
Keywords: Glioma, Astrocytoma, Hemorrhage, Edema, Intracranial Hypertension, (Source: MeSH NLM)
Aesthetic and psychological outcomes of cranioplasty, polymethyl methacrylate versus titanium mesh
ESSAM M. YOUSSEF, MD, DINA A. SELEEM, MD, MOHAMED A. YAHIA, MD
Abstract (Spanish) ||
Full Text ||
PDF (English)
ABSTRACT
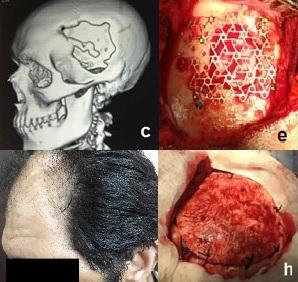
Introduction: Problems with appearance may negatively affect the mental health of individuals with disfigurement so, cranioplasty has an important role in improving the physical appearance of patients as well as their psychological symptoms.
Objective: This study aims to highlight the aesthetic as well as the psychological outcomes of cranioplasty using the two most widely used synthetic graft materials; polymethyl methacrylate (PMMA) and titanium mesh.
Methods: This is a prospective study conducted on patients with apparent skull deformity who underwent cranioplasty using PMMA or titanium mesh from April 2016 to April 2017 and were followed up for one year. Patients were assessed preoperatively, at three months, and one year postoperatively using the Derriford Appearance Scale 24 (DAS 24) and the Hospital Anxiety and Depression scale (HADS).
Results: 42 patients; 25 males and 17 females were recruited. PMMA was used in 23 patients while titanium mesh was used in 19 patients. There were no significant differences regarding early and late complications between both groups. Revision surgery was necessary in only four cases having equal rates between both groups. There was a marked reduction in DAS 24 and HADS scores postoperatively with better scores in the PMMA group especially at three months after cranioplasty.
Conclusion: Cranioplasty had positive effects on patients' distress regarding their appearance and their psychological symptoms. PMMA had better parameters than titanium mesh. Both PMMA and titanium mesh had comparable aesthetic outcomes with no statistically significant difference regarding the complication rates.
Keywords: Cranioplasty, Polymethyl methacrylate, Titanium, Physical Appearance, Body, Depression (source: MeSH NLM)
Impact of the COVID-19 pandemic on patients with rupture of intracranial aneurysm at the Dos de Mayo National Hospital in Lima Peru
JOSÉ LUIS ACHA S., JULIO JOSYMAR QUISPE D.
Abstract (Spanish) ||
Full Text ||
PDF (Spanish) ||
PDF (English)
ABSTRACT
|
Objective: To evaluate the impact on the outcome of patients with a ruptured aneurysm, who are admitted to the Dos de Mayo National Hospital in the context of the COVID-19 pandemic.
Methods: 42 operated for ruptured aneurysms were included in the context of the COVID-19 pandemic between March 1 and December 31, 2020 (group A), and a control group of 44 patients operated on between March 1 and December 31, 2019 (group B). Upon admission, the poor neurological status defined by the WFNS> 3, the Fisher IV high-grade tomographic status with intracerebral hematoma or acute hydrocephalus, which required external ventricular drainage (EVD), and the presence of vasospasm were evaluated. The Modified Rankin Scale was evaluated at discharge. Statistical analysis was performed to compare both groups.
Results: The rates of poor neurological presentation and complications during the presurgical evolution (intracerebral hemorrhage and acute hydrocephalus that required EVD) were higher in group A (p = 0.002 and p <0.05, respectively). The delay in the admission of the patient to the emergency room to receive treatment was 7.5 days in group A and 4.95 days for group B. All these factors contributed to a lower possibility of recovery in group A, which was correlated with higher Values on the Modified Rankin Scale at discharge for this group (p = 0.04).
Conclusion: We did not find national reports on ruptured aneurysms treated in the context of the pandemic, this being one of the first studies that demonstrate the impact of the COVID-19 pandemic in patients with ruptured intracranial aneurysm. The population should be educated on how to act in case of specific symptoms such as sudden intense headache, neurological deficit, or acute chest pain, which should receive timely care, immediate referral, and priority of treatment in referral hospitals in order to reduce morbidity and mortality of complex neurological pathologies.
Keywords: Intracranial Aneurysm, Aneurysm, Ruptured, Cerebral Hemorrhage, Pandemics, COVID-19. (Source: MeSH NLM)
|
Mild cranioencephalic trauma in the child population. Experience at the Baca Ortiz Hospital, Quito-Ecuador, 2016-2019
ANDREA PAEZ T., ALICIA TORRES M., ADRIANA GONZÁLEZ G., RODOLFO BERNAL C., JESÚS CASTRO V.
Abstract (Spanish) ||
Full Text ||
PDF (Spanish) ||
PDF (English)
ABSTRACT
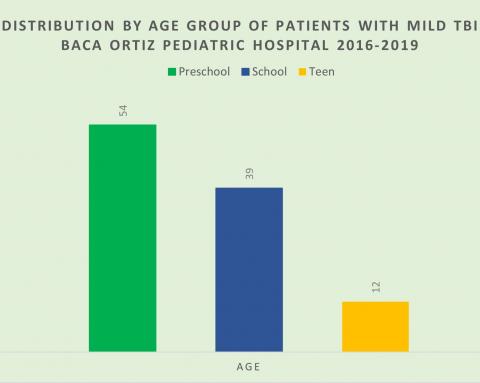
Introduction: The alteration at the anatomical and/or functional level, both motors, sensory and cognitive, a product of the sudden exchange of mechanical energy caused by an external force on the skull, is what defines a traumatic brain injury (TBI). The permanence or transience of these alterations determines the severity of the TBI, with 70 to 80% of a mild type whose neurological symptoms are of little intensity and duration. Clinical observation in mild TBI includes observing children under 2 years of age with trauma without fracture or admission criteria clinically for 2 to 4 hours and observing children with symptoms or mechanism of fall for 4 to 6 hours not known. The objective of the study is to describe mild TBI at Baca Ortiz Pediatric Hospital, a national children's referral hospital in Ecuador, during the period from January 2016 to December 2019.
Methods: Cross-sectional, descriptive, and retrospective study that includes patients diagnosed with mild head trauma evaluated and treated in the Neurosurgery Service of the Baca Ortiz Pediatric Hospital, from January 2016 to December 2019.
Results: During the period 2016 to 2019, 105 children with mild TBI were diagnosed and treated, this being more frequent in males (62.85%) and during the preschool stage (51.42%). Of all of them, 82.85% received specialty medical care in the first 6 hours after the trauma. The main etiology was the fall produced at home (66.66%).
Conclusions: Mild traumatic brain injury is one of the main reasons for pediatric hospital consultation in our setting. It mostly occurs in male patients of preschool age, because of falls at home.
Keywords: Craniocerebral Trauma, Child, Hospitals, Pediatric, Referral and Consultation (Source: MeSH NLM)
Neurological Severity Classification System (CSN-System) in adults with BTI, Hospital Cayetano Heredia, Lima - Peru, 2020. Preliminary study
ELDER CASTRO C., ROMULO RODRIGUEZ C.
Abstract (Spanish) ||
Full Text ||
PDF (Spanish) ||
PDF (English)
ABSTRACT
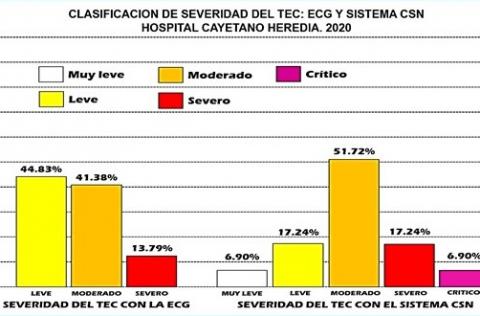
Objectives: Traumatic Brain Injury (TBI) is the disruption of brain function and architecture. The Glasgow Coma Scale (GCS) is the most widely used TBI severity classification; however, it assesses the functional status of the brain resulting from highly heterogeneous lesions and has little accuracy. The Neurological Severity Classification System (NSC System), a clinical-tomographic instrument designed to overcome lesion heterogeneity, assesses brain function and structure in determining the severity of BTI.
Methods: Observational, prospective, and cross-sectional study in adults with BTI from the emergency service of the Cayetano Heredia Hospital, April - August 2020. It included patients aged 18 years or older with acute BTI. The NSC system was compared with the GCS in the BTI classification.
Results: Of 29 patients, 82.76% were male and 82.76% were between 18 and 64 years old. The severity of the TBI through the NSC System was very mild 6.70%, mild 17.24%, moderate 51.72%, severe 17.24%, and critical 6.70%. There was an association between the NSC System and the Rotterdam Computed Tomographic Score (RCTS) (p = 0.005), a moderate positive correlation of the NSC System with the RCTS (Rho 0.6773, p = 0.0001), an association between the NSC System and the indication for neurosurgical intervention (p = 0.002), as well as high sensitivity-specificity in the distinction of severity categories with the NSC System, and lower GCS performance.
Conclusions: The NSC clinical-tomographic system improves the determination of the severity of BTI in comparison with GCS and provides an excellent relationship with the indication for neurosurgical intervention.
Keywords: Brain Injuries, Traumatic, Brain, Glasgow Coma Scale, Functional Status (Source: MeSH NLM)
Presigmoid transpetrous approach (partial petrosectomy) combined with subtemporal transtentorial approach for petroclival meningioma
FERNANDO PALACIOS S., MANUEL LAZON A., EDUARDO ROMERO V., ROMMEL RODRIGUEZ B.
Abstract (Spanish) ||
Full Text ||
PDF (Spanish) ||
PDF (English)
ABSTRACT
Introduction: Petroclival meningiomas constitute 3 to 10% of meningiomas of the posterior fossa, they originate in the petroclival fissure, in the upper part of the clivus, petrosal apex, and medial to the trigeminal nerve. Resection of these tumors is a neurosurgical challenge. The combined partial petrosectomy approach associated with a sub-temporal approach is a technique described by various authors; however, its performance is considered highly complex. We report the case of a petroclival meningioma operated successfully in our hospital using a combined presigmoid and subtemporal transtentorial transpetrosal approach.
Clinical case: 33-year-old female patient with a clinical picture of headache, nausea, and gait disturbance. Brain magnetic resonance imaging showed a large right petroclival tumor (4.2x3.9x3.8cm) that displaced the brainstem and secondary hydrocephalus. The hydrocephalus was treated with a ventricular peritoneal shunt. Then, the tumor was resected using a combined presigmoid and subtemporal transpetrosal approach, a technique that allowed adequate exposure of the tumor, achieving complete resection, without intraoperative complications. Postoperative evolution was favorable, with no sequelae.
Conclusion: The combined presigmoid and transtentorial subtemporal transpetrous approach for petroclival meningiomas is an effective and feasible technique to perform in our environment. The support of technology such as Neuronavigation, the ultrasonic aspirator, intraoperative monitoring, and adequate experience in skull base surgery are fundamental factors for the success of this surgery.
Keywords: Meningioma, Skull Base Neoplasms, Craniotomy, Neurosurgical Procedures. (Source: MeSH NLM)