SAMIR COLQUEHUANCA CH., LIZBETH CORA L., NATALI ABAD ILLACUTIPA M.
Tipo:
Case Report
ABSTRACT (English):
Introduction: Epidural hematomas are one of the most frequent complications of head injuries. Bifrontal epidural hematomas (BEH) are rare, are associated with high-intensity trauma, and are associated with high mortality. We present the clinical case of a patient with bifrontal epidural hematoma with a Glasgow Coma Scale of 6/15 on admission.
Clinical case: A 27-year-old male patient suffered a traffic accident while riding a linear motorcycle without protection, in an apparent alcoholic state. He was diagnosed with a multifragmentary depressed skull fracture and a bifrontal epidural hematoma, which extended to the temporoparietal region of the right side with a volume greater than 215cc and with a high risk of nailing. A bifrontal craniotomy and evacuation of the epidural hematoma were performed. The postoperative evolution was favorable despite a mild neurological sequela.
Conclusion: Bifrontal epidural hematoma is a rare clinical entity, and its prognosis depends on the preoperative neurological situation.
Keywords: Hematoma, Epidural, Cranial, Craniocerebral Trauma, Craniotomy (Source: MeSH NLM)
ABSTRACT (Spanish):
Introducción: Los hematomas epidurales constituyen una de las complicaciones más frecuentes de los traumatismos craneales. Los hematomas epidurales bifrontales (HEB) son poco frecuentes, se asocian a traumatismo de gran intensidad y se acompañan de elevada mortalidad. Presentamos el caso clínico de un paciente con hematoma epidural bifrontal con una Escala de Glasgow de 6/15 al ingreso.
Caso Clínico: Paciente varón de 27 años que sufrió un accidente de tránsito mientras manejaba una moto lineal sin protección, en aparente estado etílico. Fue diagnosticado de una fractura craneal multifragmentaria con hundimiento y de un hematoma epidural bifrontal, el cual se extendía a la región temporoparietal del lado derecho de un volumen superior a 215cc y con un alto riesgo de enclavamiento. Se realizó una craneotomía bifrontal y la evacuación del hematoma epidural. La evolución postoperatoria fue favorable, aunque con leve secuela neurológica.
Conclusión: El hematoma epidural bifrontal es una entidad clínica poco frecuente y su pronóstico depende fundamentarme de la situación neurológica preoperatoria.
Palabras Clave: Hematoma Epidural Craneal, Traumatismos Craneocerebrales, Craneotomía (Fuente: DeCS Bireme)
INTRODUCTION
Epidural hematomas (EH) are a common complication of head injuries.1 They generally affect young patients and have a higher incidence in the frontotemporal region.2 Traffic accidents are the main culprits in middle-income countries and low, which are generally also the most populated. 3
Its location is usually unilateral, having published cases of bilateral hematomas whose presentation can be simultaneous or successive. On other occasions, an EH appears as a complication of previous surgical procedures performed in a contiguous or distant region, which can also be bilateral.1
In this report, we present the case of an extensive bifrontal epidural hematoma (BEH) in a 27-year-old patient with a type III Marshal scale diffuse lesion.
CLINICAL CASE
History and examination: A 27-year-old male patient with an illness time of approximately 12 hours, who was referred to Juli's hospital, for having suffered a traffic accident while driving a linear motorcycle, without protection, in an apparent alcoholic state, falling into a well where it is found by relatives hours later. On physical examination: Patient unconscious, on a 9 Glasgow Coma Scale, preserved ipsilateral and contralateral photomotor reflex; Protopathic and epicritic sensitivity preserved, muscle strength 5/5 in the left half body and hemiplegia in the right half body. The scalp had a solution of continuity at the level of the frontoparietal region of the left side, with a length of 10cm and a depth of approximately 1cm. On palpation, he presented pain of moderate-intensity and depression in this region.
A non-contrast cerebral tomography (CT) with bone window and 3D reconstruction was performed, which showed a multifragmentary fracture with cranial subsidence in the left frontoparietal region, one of the fragments was embedded in the brain parenchyma causing a cerebromeningeal laceration; A bifrontal epidural hematoma was also evidenced, extending to the temporoparietal region on the right side. (Fig. 1 and 2)
|
Fig 1. (A) Brain CT without contrast (parenchymal window) showing a bifrontal epidural hematoma, extending to the temporoparietal region on the right side. (B, C) Brain CT (bone window), showing a depressed multifragmentary fracture in the left frontoparietal region, with one of the fragments embedded in the brain parenchyma causing a contusion and cerebral edema.
|
|
Fig 2. Brain CT without contrast (parenchymal window) showing in (A, B, C) a hyperdense crescent-shaped lesion corresponding to a bifrontal epidural hematoma that extends to the temporoparietal region of the right side, measuring 10 cm high, 20cm long, and 2cm wide. The volume of the hematoma according to the formula ABC / 2 = 215cc (where “A” is the maximum length, “B” is the maximum extension of the hematoma and “C” is the thickness of the hemorrhage).
|
The patient was diagnosed with multiple traumas with severe head trauma, bilateral frontotemporoparietal epidural hematoma, open skull fracture with the sinking of the left frontoparietal skull, and severe acute cerebral edema. Being in Glasgow: 6/15 is scheduled for emergency surgery.
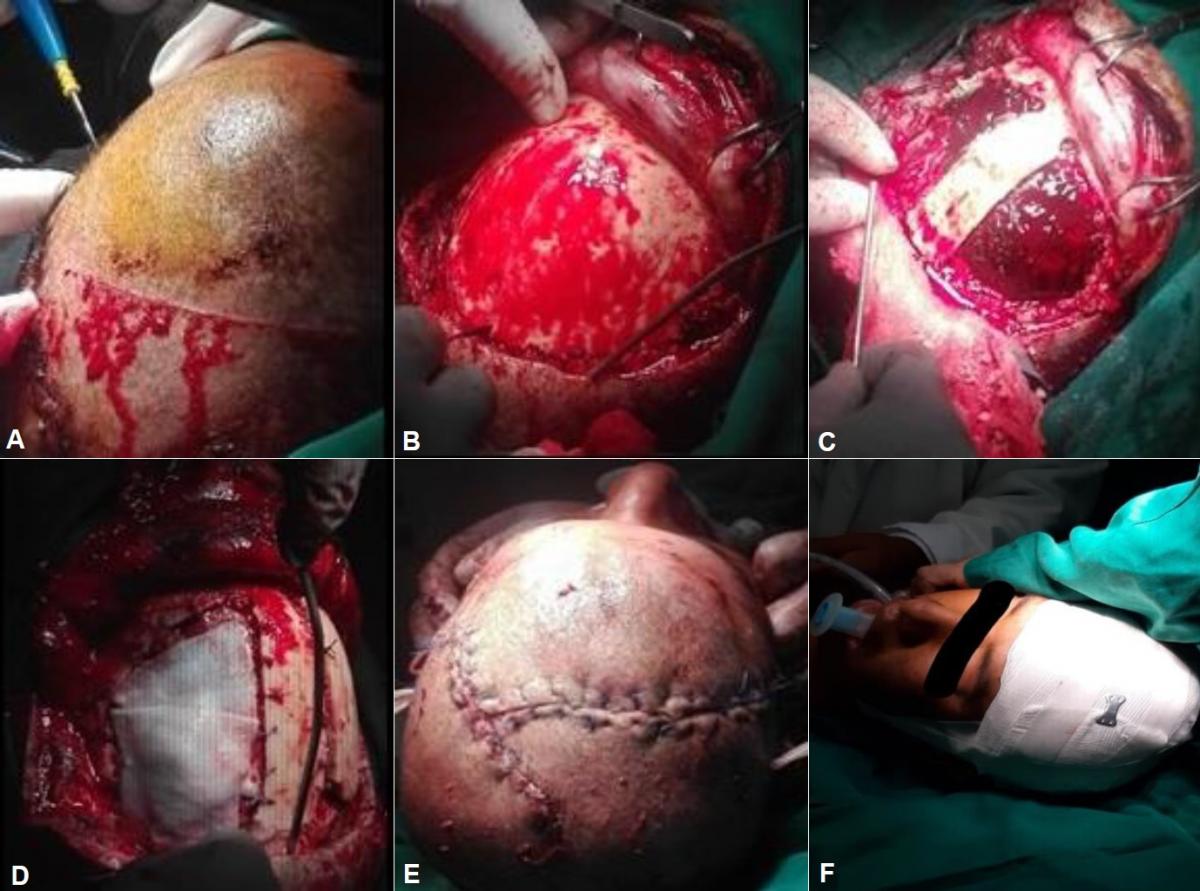
Surgical treatment: A bilateral frontal craniotomy, squirlectomy was performed and the epidural hematoma was evacuated in its entirety. Underlying cerebral contusion and great cerebral edema were evidenced, which produced protrusion of the brain tissue. Dura repair and duroplasty were performed, leaving a drain in the operative bed. It is sutured in 3 planes and a Penrose drain is left. (Fig 3)
|
Fig 3. Intraoperative images showing the evacuation of the bifrontal epidural hematoma. (A) Bicoronal incision. (B) Exposure of frontal bone. (C) Bifrontal craniotomy with bone preservation in the midline. Bilateral epidural hematoma can be seen. (D) Dura graft after the evacuation of the hematoma. (E) Skin and soft tissue closure (double path is seen due to previously sutured skin wound) (F) Patient at the end of surgery.
|
Clinical evolution: On the first postoperative day the patient did not respond to the questioning, the tone was lowered, and he presented few spontaneous movements to the painful stimulus, the Glasgow Scale was 9/15. He received anti-cerebral edema treatment with mannitol, anticonvulsant prophylaxis, broad-spectrum antibiotics, and sedation, in addition to local measures to control intracranial hypertension such as elevation of the head in 30 degrees. In the following days, the evolution was slowly favorable with progressive improvement in neurological status, although with the presence of right hemiparesis with a predominance of the lower limb and speech disorder, Glasgow 12/15 scale. On 11/12/19 the family members requested voluntary discharge.
DISCUSSION
Intracranial epidural hematomas are generally unilateral, and those that present bilaterally are rare. The first intervention on a bilateral epidural hematoma was performed by James Hill in 1772 with the complete recovery of the patient. The second case corresponds to a patient operated on by G. C. Roy in 1884 for a left epidural hematoma, in which the patient died, and a hematoma was also found on the right side. 1
According to Gelaberd V. Gonzales "Bifrontal epidural hematomas constitute 2.5% of epidural hematomas operated on surgically, representing in most series between 2% and 15% of adult epidural hematomas".1 Other authors such as Subrahmanian et al. 2 "reported 22.4%", and even reaching 24.6%. On the other hand, according to Bozbuga et al. clinically, loss of consciousness is more severe in bifrontal epidural hematomas than in unilateral epidural hematomas.3
In our case, the patient at the time of admission to the emergency room presented a 6/15 Glasgow coma scale (ECG) and this finding was in correlation with that found by the author Frank et al. that “only 2% of patients with bifrontal epidural hematomas present ECG> 8. The prognosis of these patients would not be favorable because the loss of consciousness is severe. 4
However, other authors such as Gelaberd V. Gonzales,1 mention that 33.4% had an ECG greater than 8, and the author Dharker et al. 5 mentions that 70% have ECG> 8, suggesting that the loss of consciousness is not severe, and therefore the prognosis is favorable.
Understanding the mechanism of trauma provides crucial information for understanding injury. Our patient suffered a traffic accident on his linear motorbike falling into a well of approximately 2 ½ meters, impacting with it in the frontotemporoparietal region, which allows us to conclude with complete safety that this was the cause of the skull fracture and intracranial injuries.
Depending on their formation, bilateral bifrontal epidural hematomas can be acute or subacute (late). Subacute hematomas are the most frequent, according to the Frank et al. Review. They occur because the impact force is anteroposterior in 75% of cases and lateral in 25%. Contrary to what happens in unilateral epidural hematomas, the direction of the impact force is 80% lateral. In acute bifrontal epidural hematomas, the impact forces act in several directions.4 Accordingly, we suggest that, in the present case, the bifrontal epidural hematoma was acute because the patient presented a multifragmentary subsidence fracture, one of the fragments was found embedded in the brain parenchyma causing a cerebromeningeal laceration and a cerebral contusion in the left frontoparietal region.
A. Karasu et al, recommend for treatment to perform an immediate CT scan in case of head injury, especially if there is a subsidence fracture, as was done in our patient, since an early diagnosis of bifrontal epidural hematoma and early evacuation, provide excellent recovery. 6
To determine whether a patient requires surgical treatment or not, the following surgical indications for an epidural hematoma are considered: The presence of focal signs of mass effect, asymptomatic patient, but with a hematoma greater than 30cc, 8 thickness of the lesion more than 15 mm or a midline deviation more than 5 mm, 7 signs of herniation, cardiorespiratory abnormality, anisocoria with a Glasgow less than 9 and hematomas equal to or greater than 3 cm in diameter. The origin of the hematoma, the relationship of the hematoma with the adjacent structures, must also be considered. 9
In the case of our patient, he met most of the high-risk criteria, mainly having a volume of 215 ml of bifrontal hematoma, 2.5 mm midline deviation, contact with the superior longitudinal sinus. On the other hand, some authors mention that in adult patients with a Glasgow Scale between 9 and 15, epidural hematoma thickness <15 mm, hemorrhagic volume <30 ml, and midline deviation <5mm, it is recommended to keep under observation. Upon meeting the surgical criteria, our patient underwent surgery, performing a bilateral frontal craniotomy (with the extraction of multiple fragments) and total evacuation of the epidural hematoma. During the surgery, contusion and cerebral liquefaction were evidenced, which explains the edema and increased intracranial pressure that caused protrusion of the left frontoparietal brain mass and which led to a repair of the dura mater and a duraplasty.
The general prognosis of epidural hematomas is good with mortality figures that, in most cases, are below 10%, even in patients operated on in a coma. In bifrontal epidural hematomas, the prognosis is not favorable, and the figures range from 15% to 20% and some authors even mention higher figures. Mainly due to a greater degree of neurological deterioration and the existence of serious associated injuries, both cranial and brain.10 However, our patient, despite being operated on 4 days after the accident, survived the surgery, although he presented hemiplegia of the right hemibody which in the following days partially remitted mainly in the upper right limb.
CONCLUSION
Bifrontal epidural hematoma (bilateral) is a rare lesion, the loss of consciousness being more severe than in unilateral ones, in addition to the fact that mortality is also higher, and the prognosis is less encouraging.
The present case was an acute BEH, due to the characteristics of the fracture, hematoma, and involvement of the brain parenchyma. A favorable neurological evolution was observed during the time of hospitalization until the moment of voluntary discharge requested by the relatives.
REFERENCES
- Gelabert-González M., Iglesias-País M., Serramito-García R., Fernández-Villa J., García-Allut A., Martínez-Rumbo R. Hematomas epidurales bilaterales simultáneos. Neurocirugía [Internet]. 2005 jun [citado 2021 Abr 25]; 16 (3): 256-260. Disponible en: http://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S1130-14732005000300003&lng=es.
-
SubrahmanianM.V., Rajendraprasad, G.B., Rao, B.D.: Bilateral extradural haematomas. Br J Surg 1975; 62: 397- 400.
-
Bozbuga, M., Izgi, N., Polat, G., Gürel, l.: Posterior fossa epidural haematomas: observations on a series of 73 cases. Neurosurg Rev 1999; 22: 34-40.
-
Frank, E., Berger, T.S., Tew, J.M.Jr.: Bilateral epidural hematoma. Surg Neurol 1982; 17: 218-222.
-
Dharker, S.R., Bhargava, N.: Bilateral epidural haematoma. Acta Neurochir (Wien) 1991; 110: 29-32.
-
Karasu A, Civelek E, Aras Y, Sabanci PA, Cansever T, Yanar H, et al. Analyses of clinical prognostic factors in operated traumatic acute subdural hematomas. Ulus Travma Acil Cerrahi Derg. 2010; 16: 233–6.
-
Kothari RU, Brott T, Broderick JP, Barsan WG, Sauerbeck LR, Zuccarello M, et al. The ABCs of measuring intracerebral hemorrhage volumes. Stroke. 1996.
-
Kothari RU, Brott T, Broderick JP, Barsan WG, Sauerbeck LR, Zuccarello M, et al. The ABCs of measuring intracerebral hemorrhage volumes. Stroke. 1996.
-
Guidelines for minor head injured patients’ management in adult age. The Study Group on Head Injury of the Italian Society for Neurosurgery. J Neurosurg Sci. 1996 Mar; 40(1): 11-15.
-
F. AlberdiI. García L. Atutxa M. Zabarte. Grupo de Trabajo de Trauma y Neurointensivismo de Epidemiología del trauma grave. Volume 38, Issue 9, December 2014, Pages 580-588.
__________________________________________________________
Disclosures
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Authors Contributions
Conception and design: All authors. Drafting the article: Colquehuanca. Critically revising the article: Colquehuanca, Cora, Illacutipa. Reviewed submitted version of manuscript: Colquehuanca. Approved the final version of the manuscript on behalf of all authors: Colquehuanca.
Correspondence
Samir Colquehuanca Chuquija. Scientific Association of Medical Students (ACEM – UNA) Puno, Peru. National University of the Altiplano (UNA). 1153 Floral avenue, Puno 21001, Peru. E- mail: diablitomelas@gmail.com